
Getting What We Pay For: Innovations Lacking in Provider Payment Reform for Chronic Disease Care
HSC Research Brief No. 6
June 2008
Ann Tynan, Debra A. Draper
Despite wide recognition that existing physician and hospital payment methods used by health plans and other payers do not foster high-quality and efficient care for people with chronic conditions, little innovation in provider payment strategies is occurring, according to a new study by the Center for Studying Health System Change (HSC) commissioned by the California HealthCare Foundation. This is particularly disconcerting because the nation faces an increasing prevalence of chronic disease, resulting in continued escalation of related health care costs and diminished quality of life for more Americans. To date, most efforts to improve care of patients with chronic conditions have focused on paying vendors, such as disease management firms, to intervene with patients or redesigning care delivery without reforming underlying physician and hospital payment methods.
While there is active discussion and anticipation of physician and hospital payment reform, current efforts are limited largely to experimental or small-scale pilot programs. More fundamental payment reform efforts in practice are virtually nonexistent. Existing payment systems, primarily fee for service, encourage a piecemeal approach to care delivery rather than a coordinated approach appropriate for patients with chronic conditions. While there is broad agreement that existing provider payment methods are not well aligned with optimal chronic disease care, there are significant barriers to reforming payment for chronic disease care, including (1) fragmented care delivery; (2) lack of payment for non-physician providers and services supportive of chronic disease care; (3) potential for revenue reductions for some providers; and (4) lack of a viable reform champion. Absent such reform, however, efforts to improve the quality and efficiency of care for chronically ill patients are likely to be of limited success.
- Growing Burden of Chronic Disease
- Flawed Payment Methods
- Payment-Reform Experiments and Pilots
- Payment Reforms in Conceptual Stage
- Barriers to Reforming Provider Payment
- Implications
- Notes
- Data Source and Funding Acknowledgement
Growing Burden of Chronic Disease
![]() hronic diseases—such ongoing conditions as asthma,
diabetes and heart disease—are among the most prevalent and costly of all
illnesses in the United States. In 2005, an estimated 133 million people had
at least one chronic disease—a figure projected to increase to 171 million people
by 2030.1 People with chronic diseases account for a disproportionate
share of the nation’s health care costs. According to the Centers for Disease
Control and Prevention (CDC), chronic diseases account for 70 percent of all
deaths in the United States and 75 percent of the nation’s $2 trillion annual
medical care costs. Further, chronic conditions cause major limitations in activity
for more than one in every 10 Americans, or 25 million people, according to
the CDC. Such limitations can affect individuals’ quality of life, as well as
workforce productivity. A 2007 American Hospital Association report, for example,
estimated that three chronic diseases—asthma, diabetes and high-blood pressure—result
in 164 million days of absenteeism each year, costing employers $30 billion.
hronic diseases—such ongoing conditions as asthma,
diabetes and heart disease—are among the most prevalent and costly of all
illnesses in the United States. In 2005, an estimated 133 million people had
at least one chronic disease—a figure projected to increase to 171 million people
by 2030.1 People with chronic diseases account for a disproportionate
share of the nation’s health care costs. According to the Centers for Disease
Control and Prevention (CDC), chronic diseases account for 70 percent of all
deaths in the United States and 75 percent of the nation’s $2 trillion annual
medical care costs. Further, chronic conditions cause major limitations in activity
for more than one in every 10 Americans, or 25 million people, according to
the CDC. Such limitations can affect individuals’ quality of life, as well as
workforce productivity. A 2007 American Hospital Association report, for example,
estimated that three chronic diseases—asthma, diabetes and high-blood pressure—result
in 164 million days of absenteeism each year, costing employers $30 billion.
People with chronic conditions, particularly those with more than one chronic disease, typically receive care from multiple providers and take multiple prescription medications. Consequently, there is increased risk for duplication of services and tests, avoidable hospitalizations and adverse drug reactions. Optimal care for people with chronic diseases involves coordinated, continuous treatment by a multidisciplinary team of health care professionals. For example, for a patient with diabetes and severe congestive heart failure, having the primary care physician and nursing staff coordinate with the patient’s cardiologist about disease status and medication regimen would be beneficial. Similarly beneficial would be diabetes education from a nurse or peer educator to provide important tools for patient self-management and connecting patients to community resources to support other social, behavioral, mental health and home health needs that may impact overall health.
However, existing health care delivery and payment systems are largely organized to support the diagnosis and treatment of acute, or episodic, conditions. The result is often fragmented, ineffective and costly care for people with chronic diseases.2 The Chronic Care Model, a model for care delivery developed by the Group Health MacColl Institute for Healthcare Innovation, recommends essential elements of a health care system that encourages high-quality disease care, including: 3
- A culture, organization and mechanisms that promote high-quality care;
- A delivery system with clearly defined staff roles, patient-care tasks and follow up incorporated into standard procedures;
- Decision-support to allow treatment based on evidence-based care guidelines and integration of specialty and primary care;
- Clinical information systems, such as disease registries, that provide timely access to patient information;
- Support for patient self-management; and;
- Community relationships to mobilize resources to help meet patients’ needs.
While there is widespread acknowledgement that current provider payment methods do not encourage efficient or effective delivery of chronic disease care and despite considerable discussion about reforming payment, actual payment reforms have been virtually nonexistent, according to interviews with executives of national health plans, Blue Cross Blue Shield (BCBS) plans, and regional/local health plans, as well as employer groups and other relevant organizations (see Data Source).
Back to Top
Flawed Payment Methods
![]() ccording to the Institute of Medicine, “Fundamental changes
in approaches to health care payment are necessary to remove impediments to
and create incentives for significant quality improvement.”4
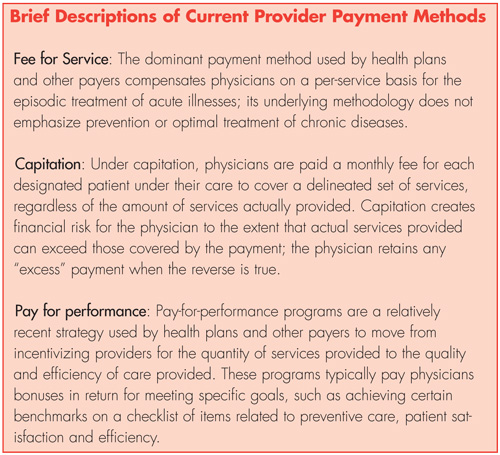
Existing methods used by health plans and others to pay providers for chronic
disease care are largely the same as those used to pay for care more generally.
These methods—primarily fee for service and, to a much lesser extent, capitation,
where providers receive fixed per-patient, per-month payments—are not well aligned
with the delivery of optimal chronic disease care. Pay-for-performance initiatives,
while providing incentives for quality improvement on measures that are largely
related to chronic disease care, are not designed to achieve comprehensive payment
reform for chronic disease care. (See box below for information on existing
payment methods.)
ccording to the Institute of Medicine, “Fundamental changes
in approaches to health care payment are necessary to remove impediments to
and create incentives for significant quality improvement.”4
Existing methods used by health plans and others to pay providers for chronic
disease care are largely the same as those used to pay for care more generally.
These methods—primarily fee for service and, to a much lesser extent, capitation,
where providers receive fixed per-patient, per-month payments—are not well aligned
with the delivery of optimal chronic disease care. Pay-for-performance initiatives,
while providing incentives for quality improvement on measures that are largely
related to chronic disease care, are not designed to achieve comprehensive payment
reform for chronic disease care. (See box below for information on existing
payment methods.)
One respondent described the underlying flaws of existing payment methods as “fee for service encourages physicians to do as much as they can for as many as they can, and capitation encourages physicians to do as little as they can for as many as they can.” Fee for service rewards high volume and, as a result, can create incentives for overuse and duplication of services.5 Fee for service does not typically pay physicians and/or their staff for coordinating with other providers or for providing patient education, patient group visits, and phone and e-mail communications for patient care outside of the traditional physician office visit—often critical components of an effective treatment regimen for patients with chronic conditions.6
While capitation has the potential to better support chronic disease care, these methods are not widely used. Capitation payments were initially envisioned as a means to reward coordinated and efficient care delivery with an emphasis on prevention and primary care—elements that would benefit patients with chronic conditions. Capitation theoretically encourages cooperation among physicians and other providers and allows physician organizations the flexibility to allocate funds to support activities beneficial to chronic disease care, such as care coordination and patient education.7
But capitation also has drawbacks—it can create perverse incentives for physicians to inappropriately withhold services or, unless payments are appropriately risk adjusted, to avoid caring for complex, high-cost patients, such as those with chronic conditions.8 According to one health plan executive, “Any group doing full-risk capitation [in which the physician is at financial risk for all services, including inpatient care and prescription drugs] has all of the right incentives to figure out how to do a good job managing people with chronic conditions.” However, payers that continue to use capitation most often use professional risk capitation where the financial risk is limited only to services provided directly by physicians.
Pay-for-performance programs aim to address some of the weaknesses of current payment methods by rewarding physicians with additional payment for providing high-quality care. While these programs are growing in prevalence, just over one-quarter of primary care physicians report having quality-based performance incentives.9 Further, most current pay-for-performance programs were never intended as a comprehensive approach to provider payment for chronic disease care and fail to address such issues as the lack of payment for care coordination for chronically ill people or actively engaging non-physician practitioners in care delivery.
Back to Top
Payment-Reform Experiments and Pilots
![]() lthough many respondents were unaware of any payment-reform experiments or pilot programs, others were able to identify and discuss several small-scale programs and one initiative just getting underway. For many of these efforts, however, changing care delivery was the primary impetus of the initiative; changes in payment methods were not always explicit components. These efforts are important to examine because, although they are relatively small, they provide critical insights into the current state of payment reform or lack thereof; they also offer key insights into the difficulties associated with reform. But because most of these efforts are experiments or early pilot projects, it is too soon to conclude what impact, if any, they have on quality, patient outcomes or costs. Also unclear is the extent to which these efforts may be replicable in other settings or feasible on a larger scale. Examples of efforts identified by respondents include the:
lthough many respondents were unaware of any payment-reform experiments or pilot programs, others were able to identify and discuss several small-scale programs and one initiative just getting underway. For many of these efforts, however, changing care delivery was the primary impetus of the initiative; changes in payment methods were not always explicit components. These efforts are important to examine because, although they are relatively small, they provide critical insights into the current state of payment reform or lack thereof; they also offer key insights into the difficulties associated with reform. But because most of these efforts are experiments or early pilot projects, it is too soon to conclude what impact, if any, they have on quality, patient outcomes or costs. Also unclear is the extent to which these efforts may be replicable in other settings or feasible on a larger scale. Examples of efforts identified by respondents include the:
- BCBS of North Dakota nurse care management pilot;
- Rhode Island Medicaid Connect Care Choice Program;
- BCBS of Massachusetts alternative provider contracting approach;
- Ambulatory Intensive Caring Unit; and
- Medicare Physician Group Practice demonstration.
These efforts provide illustrative examples of several different—albeit not necessarily new or novel—approaches to provider payment and incentives. The first two efforts use financial incentives, including additional payment, to encourage physicians to enhance their capacity around chronic disease care; the next two efforts use a payment mechanism (global fee or salaried arrangement) that provides physicians the flexibility to allocate payment across providers and care settings based on an individual patient’s needs; and, the last effort uses additional payment to reward physicians that demonstrate improvement in the quality and efficiency of care provided.
BCBS of North Dakota Nurse Care Management Pilot
In 2005, BCBS of North Dakota implemented a one-year, provider-based diabetes disease management pilot program in collaboration with an integrated delivery system. BCBS provided the system a $20,000 grant to help support the salary of a nurse case manager and to assist with other start-up expenses. The plan also agreed to share a portion of any cost savings from the initiative with the system.
Diabetic patients in a designated study clinic received disease management intervention services from the nurse case manager and other staff located in the physician practice. The intervention services consisted of a patient history review, development of a care plan, monitoring/tracking of care needs, teaching self-management skills, patient meetings with a nurse case manager to assist in medication comprehension, encouragement of appropriate preventive testing, and generally responding to patients’ needs and questions. Patient outcomes and health care costs were then compared to diabetic patients who did not receive these services.
The results of the pilot reportedly were positive. Hospital admissions and emergency department visits decreased for diabetic patients who received disease management services compared with those who did not. After removing outliers, BCBS calculated that the total mean savings from 2003 (the baseline year) and 2005 (the intervention year) between the two clinics was approximately $300,000; savings were shared between the plan and the system.
Based on the perceived success of the diabetes pilot program, BCBS expanded the project to four other clinics and two other chronic conditions—high-blood pressure and heart disease. The plan expects to implement a $175 per-member, per-year payment to physicians of patients participating in the disease management intervention, in addition to sharing half of any cost savings—less the yearly fees—with physicians. BCBS will continue to pay fee for service for all other services.
Several characteristics of health care delivery in North Dakota, however, may preclude replication of this program in other settings. North Dakota is a sparsely populated state with largely vertically integrated provider systems—there are about six provider organizations (including hospitals) that represent almost 90 percent of all physician and hospital care provided in the state. Further, BCBS of North Dakota is the dominant insurer in the state, with approximately 90 percent of the commercial business in the state.
Rhode Island Medicaid Connect Care Choice Program
The Connect Care Choice program is a primary care case management program for adults with multiple chronic conditions (not also eligible for Medicare) who are enrolled in Rhode Island’s fee-for-service Medicaid program. The program’s goal is to promote primary care in community-based settings, including physicians’ private practices, community health centers and hospital outpatient clinics. To participate in the program, physician practices must meet the patient-centered medical home criteria jointly defined by the American College of Physicians, American Academy of Family Physicians, American Academy of Pediatrics and American Osteopathic Association,10 which requires the primary care provider to:
- Partner with patients to manage and coordinate their health care, including behavioral health;
- Incorporate the Chronic Care Model to help chronically ill patients manage their conditions and prevent avoidable complications by providing well and preventive care visits, self-management support and education;
- Use a dedicated nurse care manager either in the practice or provided to the practice from the community; and
- Use scheduling systems that minimize appointment delays—focusing on either same-day or after-hours appointments.
Physician practices that meet the patient-centered medical home criteria and use electronic medical records (EMRs) are paid a $10 per-member, per-month fee for treating chronically ill adults in Medicaid fee for service enrolled in the Connect Care Choice Program; practices without an EMR that meet the patient-centered medical home criteria are paid $5 per member, per month. The program also pays for a nurse case manager to work cooperatively with physicians onsite in the practice to help support enrolled patients. Since Rhode Island Medicaid payment rates were among the lowest in the country, the state concurrently increased reimbursement for certain primary care visits for Connect Care Choice program enrollees. The program began enrolling patients and physician practices in September 2007 and plans to rely on savings from avoidable hospitalizations and emergency department visits to fund the program.
BCBS of Massachusetts Alternative Physician Contracting Approach
In early 2008, BCBS of Massachusetts introduced an alternative contracting—and payment—approach for physicians. The BCBS approach uses a risk-adjusted annual global payment, including payment for all inpatient hospitalizations, physician visits, labs, radiology testing, ancillary services, home health, and skilled-nursing facility care. Physicians who meet certain quality targets are eligible for a performance payment of up to 10 percent of the annual global payment. This approach is currently geared toward physicians participating in the plan’s health maintenance organization (HMO) products who also have existing relationships with integrated care delivery systems.
BCBS of Massachusetts officials said that the performance payment is based on process and outcome measures of chronic disease care. Plan officials noted that this type of contracting approach is intended to address some of the barriers associated with providing optimal chronic disease care, such as the of lack of payment for care coordination, because it gives providers the flexibility to allocate payment across different providers and care settings and provides incentives to care for complex patients. This contracting approach relies on an attribution model to identify which patients belong to which providers, which can be more easily accomplished in an HMO where enrollees have designated primary care physicians rather than in a preferred provider organization (PPO) where this is not required. It is unclear how prevalent this contracting arrangement will ultimately be or how agreeable physicians will be to the terms because negotiations with physician groups were in the early stages.
Ambulatory Intensive Caring Unit
One respondent pinned hopes for payment reform on “something drastic like going to the salary model or something to get people’s attention to something worth trying.” The Ambulatory Intensive Caring Unit (A-ICU) approach supports redesigned care delivery using a multidisciplinary team of salaried health care providers in a dedicated clinic setting to improve the quality of care, as well as to reduce the costs of care, for chronically ill, high-cost patients.
The increased costs—primarily provider salaries and increased intensity of services—are expected to be offset by savings that are expected to begin accruing 12-36 months after start up. The A-ICU model is geared toward organizations that assume global insurance risk for high-cost patients, such as self-funded employers and union trust funds. Applicability of this model is likely limited to these large self-funded settings where the employer or group also has the financial wherewithal to undertake such an initiative. A large employer group in Seattle and a union trust fund in Atlantic City, in collaboration with provider organizations, launched pilot programs testing this approach in 2007.
Medicare Physician Group Practice Demonstration
In recent years, Medicare has launched several demonstration projects focusing on chronically ill people. While respondents acknowledged these efforts focused on chronic disease care, most Medicare demonstrations do not have a specific “new” or “innovative” provider payment component. Rather, they have largely focused on redesigning care delivery or paying vendors, such as disease management firms, to intervene with patients. One exception is the Medicare Physician Group Practice Demonstration, which offers large physician group practices (200 or more physicians) the opportunity for “shared savings” with Medicare for improving the quality and efficiency of care of Medicare fee-for-service beneficiaries. Participating practices have chosen to apply care management strategies and practice-redesign processes to patients with chronic illnesses, those transitioning between care settings or those needing end-of-life care.11
Under the demonstration, physician groups continue to be paid under the Medicare fee-for-service system, and if they meet certain minimum thresholds for quality improvement and payer spending growth reductions, they can earn up to 80 percent of savings generated by enhancements in care management. Physician groups first must meet quality targets for improving care and then are measured on cost performance. If Medicare spending growth for patients in the demonstration is 2 percentage points less than spending growth for a comparison group of beneficiaries in the practice’s local market, then the practice qualifies for the bonus payment.
In the first year of the demonstration, all 10 of the participating physician practices improved the clinical management of Medicare patients with diabetes, but only two practices met the target for spending growth reduction and earned performance payments.
Back to Top
Payment Reforms in Conceptual Stage
![]() espondents also discussed other provider payment reform initiatives that are largely in the conceptual or planning stage, including patient-centered medical homes and the Prometheus Payment system.
espondents also discussed other provider payment reform initiatives that are largely in the conceptual or planning stage, including patient-centered medical homes and the Prometheus Payment system.
Patient-Centered Medical Homes
Patient-centered medical home pilot programs and demonstrations are being developed collaboratively by health plans, medical societies and employers, as well as Medicare and some Medicaid programs, and are intended to reduce dispersion of care across providers and to encourage care coordination, which are likely to benefit patients with chronic diseases. A proposal offered by the Patient-Centered Primary Care Collaborative, which includes most of the primary care medical societies, recommends a three-part model payment structure for care delivered in the patient-centered medical home that consists of the following components:12
- A risk-adjusted, monthly care coordination payment to the physician for work that falls outside of face-to-face visits and for the health information technologies needed to achieve better outcomes;
- Fee-for-service payments for office visits; and
- A performance-based component that recognizes achievement of quality and efficiency goals.
Prometheus Payment
The Prometheus Payment approach is premised on the use of evidence-based case rates (ECRs), and pilots testing this methodology are expected to begin in early 2009.13 A case rate is a single, risk-adjusted payment given to providers across inpatient and outpatient settings to care for a patient diagnosed with a specific condition. Payment amounts are based on the resources required to provide care recommended in evidence-based clinical guidelines. Providers can be assigned multiple ECRs for an individual patient, such as a person with multiple chronic conditions, with a process to eliminate potentially redundant services.
The underlying concept of the Prometheus Payment approach is that it can be “bolted on” to existing health plan claims payment systems; however, some of the respondents familiar with Prometheus, while supportive of the concept, expressed concern about the complexity and questioned the feasibility of launching it in the current environment of fragmented care delivery and multiple-payer systems. According to a national health plan medical director, Prometheus “is a complex system of payment and it seems to simply substitute one complex payment system for the complex payment system we already have. While the one we have doesn’t work so well, at least we’re familiar with it, and there is no real evidence that the new system will work any better.”
Back to Top
Barriers to Reforming Provider Payment
![]() hile there is broad agreement that current provider payment methods are not well aligned with optimal chronic disease care, there are significant barriers to reforming payment for chronic disease care. These include: (1) fragmented care delivery; (2) lack of payment for non-physician providers and services supportive of chronic disease care; (3) potential for revenue reductions for some providers; and (4) lack of a viable reform champion.
hile there is broad agreement that current provider payment methods are not well aligned with optimal chronic disease care, there are significant barriers to reforming payment for chronic disease care. These include: (1) fragmented care delivery; (2) lack of payment for non-physician providers and services supportive of chronic disease care; (3) potential for revenue reductions for some providers; and (4) lack of a viable reform champion.
Fragmented Care Delivery
According to one thought leader, “The needs of people with chronic conditions do not align with the health care delivery system outside of integrated delivery systems because care is fragmented and built around acute events.” Integrated delivery systems are better positioned—at least conceptually—to provide comprehensive patient care across settings with physicians, hospitals, pharmacies, and other ancillary service providers working together. Additionally, these systems have greater flexibility in allocating resources to meet patients’ needs, including those with chronic conditions. While respondents discussed that integrated delivery systems, such as Kaiser, Group Health Cooperative and the Mayo Clinic, have been the most innovative in providing chronic disease care, these systems are the minority of health care delivery settings nationally.
Care delivery is particularly problematic when it is dispersed across multiple physicians and settings, not only making it challenging to coordinate care but also making attribution difficult for payment purposes. This is particularly true for people with multiple chronic conditions who may be treated by many different practitioners. Identifying which specific physician, if any, is responsible for overseeing the care of a chronically ill patient has implications for how and what to pay physicians. Attribution is especially challenging in non-HMO insurance products because no single physician is designated as the enrollees’ primary physician. Other HSC research on care patterns has found that the average Medicare beneficiary sees two primary care physicians and five specialists, working in a median of four practices, over the course of a given year.14 Beneficiaries with chronic conditions see even more physicians—patients with four or more chronic conditions saw more than 13 physicians on average annually.15
The fragmentation of care delivery impedes the development of alternative approaches to payment that provide incentives for comprehensive and coordinated care, such as global fees and pay-for-performance incentive payments. Global fees typically include all costs for hospital, physician, and other services needed to treat an entire episode of care or for a given year for a patient with chronic conditions. Global fees are often risk-adjusted to account for differences in the severity of illness among patients. The approach relies on the distribution of the payment through the patient’s primary care physician. As one respondent noted, it is hard to develop case rates because it is hard to figure out “how to pay different providers for taking care of the patient unless all of the providers are part of an integrated delivery system.”
Lack of Payment for Non-Physician Providers and Supportive Services
Services provided outside of a face-to-face physician office visit to coordinate care, educate and follow up with patients with chronic conditions can often be performed at least as effectively and often at lower cost by providers other than physicians, such as nurses or peer educators. However, these services often are not reimbursed by Medicare.16 Since other payers frequently model payment on Medicare rules, this limitation often carries over to commercial health insurance.
According to one respondent, “We should look at nontraditional settings of care, such as the use of e-mail, phone, nursing care managers, nurse practitioners, and incentivize that.” The concept is that by redirecting more routine and less complex services to non-physician practitioners, physicians’ time would be spent managing more difficult cases. But expanding payment to non-physician services is difficult in part because of concerns that overall utilization and, therefore, costs will increase. Coverage of non-physician practitioners also may generate pushback from physicians threatened by the potential for lost revenue.
Potential for Revenue Reductions
A major goal of fundamental provider payment reform would be to encourage high-quality and efficient care, but this may result in reduced revenues for some providers. For example, care delivery initiatives that focus on people with chronic conditions often include such goals as reductions in the number of hospitalizations and emergency department visits. While these goals may result in improved quality and better patient outcomes, they are also likely to yield cost savings, which means reduced revenues, in this case, for hospitals. Efforts that result in a loss of revenues are likely to face strong resistance from affected providers, particularly those that may struggle financially because of a general decrease in volume. There is also a greater likelihood of provider pushback when the service reductions are among the more profitable services.
Lack of a Reform Champion
For any major payment reform to gain traction, it would likely have to be adopted by Medicare, the largest single payer of health care services nationally. According to one respondent, “Unfortunately, the way the system is designed in the United States, as a buyer of health care, we can only really buy what Medicare buys. to buy comprehensive care is extremely difficult.”
Several factors point to the federal government, likely through the Medicare program, as the most viable candidate to champion provider payment reform. Given its size—in terms of beneficiaries and expenditures nationally—and political significance, Medicare has considerable influence. In contrast, the private sector—with its fragmented health care purchasing structure—is less likely to be able to successfully champion a task as onerous as payment reform. The competitive nature of health plans makes them unlikely targets for a major collaboration necessary to achieve payment reform. Further, there is little impetus from employers and other health care purchasers to instigate fundamental and comprehensive provider payment reform.
Back to Top
Implications
![]() lthough it is widely recognized that current provider payment methods do not encourage high-quality and efficient chronic disease care, efforts to reform these methods generally have been limited to experiments and small pilots. There is seemingly insufficient pressure to move away from the status quo toward a more fundamental and comprehensive overhaul of current provider payment systems. Yet, this is essential as the number of people with chronic conditions and the related health care costs continue to escalate. As these pressures mount, so do the pressures to develop better ways to encourage and pay providers to deliver high-quality and cost-effective care that results in good patient outcomes.
lthough it is widely recognized that current provider payment methods do not encourage high-quality and efficient chronic disease care, efforts to reform these methods generally have been limited to experiments and small pilots. There is seemingly insufficient pressure to move away from the status quo toward a more fundamental and comprehensive overhaul of current provider payment systems. Yet, this is essential as the number of people with chronic conditions and the related health care costs continue to escalate. As these pressures mount, so do the pressures to develop better ways to encourage and pay providers to deliver high-quality and cost-effective care that results in good patient outcomes.
But it is unlikely that provider payment reform will move forward without considerably more impetus on the part of employers and other health care purchasers to overcome the inertia of the status quo. Payment reform also will be difficult without a viable and influential champion. The federal government through Medicare, although subject to intense political pressure, is likely the only entity that is in such a position. However, any major reform of Medicare provider payment is unlikely in the near future. While Medicare has conducted several recent demonstrations focusing on chronically ill people and is planning a patient-centered medical home demonstration, demonstration projects take time to execute and evaluate before wider implementation can occur. Medicare will need a mandate from the Congress to shift from developing more demonstrations to implementation—on a phased basis—of a revised payment system. This will take broad-based stakeholder support and commitment, and the desire and ability to move away from the status quo.
Back to Top
Notes
Back to Top
Data Source
HSC researchers conducted 33 semi-structured interviews with informed and knowledgeable market observers across the country between September 2007 and January 2008. Respondents included thought leaders, executive medical directors of national, BCBS, regional and local health plans, employer groups, purchasers of health care, and other observers. Interview protocols were designed with broad, open-ended questions to explore with respondents: current payment methods and incentives used by health plans and others to pay for chronic disease care (and care for other high-cost medical conditions); payment experiments and/or pilot programs; planned changes; and key considerations in reforming payment methods. The protocol design also facilitated exploration of the experimentation around payment methods and incentives and the barriers to reforming payment methods. Each interview was conducted by a two-person team of researchers, and notes were transcribed and jointly reviewed for quality and validation purposes. All interview data were coded and analyzed using the Atlas.ti qualitative software.
Back to Top
Acknowledgement: This research was funded by the California HealthCare Foundation.
ISSUE BRIEFS are published by the
Center for Studying Health System Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org