
Developing Health System Surge Capacity: Community Efforts in Jeopardy
HSC Research Brief No. 5
June 2008
Laurie E. Felland, Aaron Katz, Allison Liebhaber, Genna R. Cohen
Since Sept. 11, 2001, communities have responded to the federal call to enhance health care surge capacity—the space, supplies, staffing and management structure to care for many injured or ill people during a terrorist attack, natural disaster or infectious disease pandemic. Communities with varied experience handling emergencies are building broad surge capacity, including transportation, communication, hospital care and handling mass fatalities, according to a new study by the Center for Studying Health System Change (HSC). Communities rely on federal funding to help coordinate and plan across agencies and providers, conduct training and drills, recruit volunteers, and purchase equipment and stockpile supplies. The current federal focus on pandemic influenza has helped prepare for all types of emergencies, although at times communities struggle with fragmented and restrictive funding requirements.
Despite progress, communities face an inherent tension in developing surge capacity. The need for surge capacity has increased at the same time that daily health care capacity has become strained, largely because of workforce shortages, reimbursement pressures and growing numbers of uninsured people. Payers do not subsidize hospitals to keep beds empty for an emergency, nor is it practical for trained staff to sit idle until a disaster hits. To compensate, communities are trying to develop surge capacity in a manner that supports day-to-day activities and stretches existing resources in an emergency. Many of these efforts—including integrating outpatient providers, expanding staff roles and adapting standards of care during a large-scale emergency—require greater coordination, guidance and policy support. As time passes since 9/11 and Hurricane Katrina, federal funding for surge capacity has waned, and communities are concerned about losing surge capacity they have built.
- Communities Plan for Range of Emergencies
- Funding Drives Many Surge Capacity Activities
- Planning, Coordination Key
- Stockpiling Supplies
- Strategies to Create Space
- Stretching Staff
- Controlling Demand for Hospital Services
- Implications
- Notes
- Data Source and Funding Acknowledgement
Communities Plan for Range of Emergencies
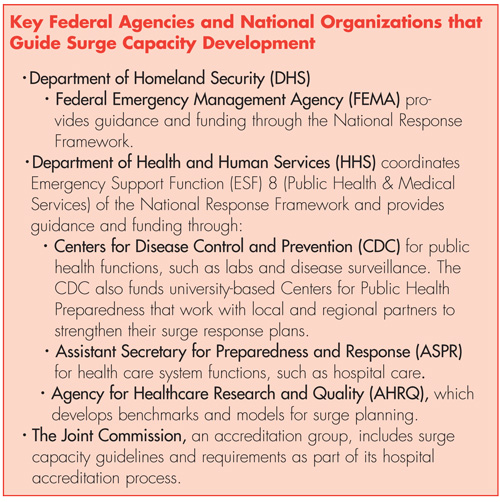
![]() Since the terrorist attacks of Sept. 11, 2001, the importance
of public health preparedness generally and surge capacity specifically—the
ability to rapidly expand to meet the greatly increased demand for medical care
and public health from large numbers of people—has been paramount to policy
makers and health care organizations. Hurricane Katrina in 2005 and other local
disasters have further highlighted the need. Federal, state and local governments
have expended considerable effort to prepare for disasters, emphasizing local
plans since local agencies and organizations are the first responders in an
emergency. Federal funding for bioterrorism preparedness, mostly directed to
state and local agencies, spiked after 9/11 (see box below
for a description of federal agencies involved in surge capacity development).1
Since the terrorist attacks of Sept. 11, 2001, the importance
of public health preparedness generally and surge capacity specifically—the
ability to rapidly expand to meet the greatly increased demand for medical care
and public health from large numbers of people—has been paramount to policy
makers and health care organizations. Hurricane Katrina in 2005 and other local
disasters have further highlighted the need. Federal, state and local governments
have expended considerable effort to prepare for disasters, emphasizing local
plans since local agencies and organizations are the first responders in an
emergency. Federal funding for bioterrorism preparedness, mostly directed to
state and local agencies, spiked after 9/11 (see box below
for a description of federal agencies involved in surge capacity development).1
Following an initial focus on intentional use of biological agents, federal funding has become more flexible to respond to a range of potential emergencies, including manmade and natural disasters. Within this “all-hazards” approach, attention to a potential pandemic influenza has increased over the past year. Concerns that avian flu could spread worldwide evoke the 1918-19 flu pandemic that killed approximately 675,000 Americans and 50 million people worldwide.2 The U.S. Department of Homeland Security has identified 14 additional scenarios to prepare for, including natural disasters, chemical, radiological, nuclear and other biological incidents.
Federal agency guidance and research are generally consistent about the main components needed for surge capacity: a management structure and communication systems, equipment and supplies, facilities, and personnel.3
Management Structure and Communication Systems. In an emergency, an overarching management structure is critical to lead the response, assign responsibilities and allocate equipment and personnel. To receive federal funding, communities must comply with the Federal Emergency Management Agency’s National Incident Management System (NIMS), which provides standards for coordinating across jurisdictions and disciplines. However, lack of clarity about which agency or sector is responsible for various components—including how each relates to the overall government command structure—can hamper a unified command.4
Equipment and Supplies. A variety of equipment, supplies and medications must be on hand for use in major emergencies to keep facilities in operation and support patient care, including specialized items for specific threats, such as anti-viral drugs for an influenza outbreak. Stockpiles and supply chains have been developed at the national, state and local levels to help provide medical and non-medical supplies during an emergency.
Facilities. During an emergency, health care providers must create additional physical space. The U.S. Department of Health and Human Services (HHS) estimates that a severe pandemic flu would require hospitalization of nearly 10 million people, yet only about 1 million staffed hospital beds are available.5 Redirecting hospital rooms from routine uses could provide additional capacity, as could planning for how to use, staff and supply non-medical buildings and temporary structures
Personnel. A large-scale emergency would require significant numbers of clinical and public health professionals to care for victims in an emergency. Yet, given workforce shortages, especially for nurses,6 hospitals need viable strategies to activate volunteers and workers from elsewhere and appropriately allocate existing staff.
Despite attention to these key components, significant concerns remain about communities’ ability to carry out a surge in capacity and their capability to attend to the specialized needs of affected people. Previous studies have suggested that surge capacity remains inadequate in the United States because of resource constraints, the challenges of inter-agency and cross-jurisdictional coordination, and multiple federal guidelines and requirements.7 Moreover, federal policy makers often lack direct relationships with communities as many federal funds are distributed through the states, and research on community-level surge capacity has been limited.
This study examines community-level surge capacity development and variation across six communities: Boston; Greenville, S.C.; Miami; Phoenix; Orange County, Calif.; and Seattle (see Data Source). To place these communities’ perspectives in a broader context with communities that have particular experience with large-scale disasters, interviews also were conducted with officials in New York City, Washington, D.C., and New Orleans, as well as with national leaders.
The communities have varied experience with large-scale emergencies, based on geography and other factors, but all consider themselves at risk. The 9/11 attacks appreciably affected New York City and Washington, D.C., although the number of people needing medical care was relatively low. Hurricane Katrina had broad and long-term impact on the New Orleans health care system—both in the numbers of people needing care and damage to medical facilities. Communities such as Miami and Orange County have been developing surge capacity for years because of the risk of natural disasters, such as hurricanes, earthquakes and wildfires. Phoenix, on the other hand, has had less exposure to natural disasters but recently heightened its focus on surge capacity given challenges serving a rapidly growing population and preparing to host several large public events in 2008.
Back to Top
Funding Drives Many Surge Capacity Activities
![]() ommunities rely heavily on federal funding for surge capacity development because state and local funding is minimal. Some funding is allocated to states or communities based on perceived risk or need, while other funding is distributed through competitive grants. Respondents reported that federal funding has raised awareness of the need for surge capacity in communities and enabled people to dedicate time to create plans, conduct drills, develop volunteer corps and purchase equipment and supplies.
ommunities rely heavily on federal funding for surge capacity development because state and local funding is minimal. Some funding is allocated to states or communities based on perceived risk or need, while other funding is distributed through competitive grants. Respondents reported that federal funding has raised awareness of the need for surge capacity in communities and enabled people to dedicate time to create plans, conduct drills, develop volunteer corps and purchase equipment and supplies.
Federal funding is fragmented, however, coming from several sources with varied requirements, making it difficult for communities to pursue a comprehensive strategy. Although respondents viewed the federal focus on pandemic flu as appropriate overall, in some cases funding restrictions preclude investment in risks seen as important locally. As a state official in Florida remarked, “Requirements and restrictions made it difficult to fit into that overarching strategy, which leaves some things we believe to be important with no funding source because each funding source has a box.” Respondents urged greater integration of various guidelines and development of meaningful and usable benchmarks to track progress across core surge capacity components. Some expressed optimism about the collaboration between the University of Pittsburgh’s Center for Biosecurity and the HHS Office of the Assistant Secretary for Preparedness and Response (ASPR) toward this end.
Further, respondents reported that funding levels are insufficient, particularly compared with the costs of developing hospital surge capacity. The Center for Biosecurity estimates that hospital costs to prepare for a pandemic well exceed ASPR funding.8 Health care financing does not support having hospital beds, equipment or workers sit idle, a fundamental tension with surge preparedness since neither public nor private payers subsidize such capacity. Reimbursement pressures and growing numbers of uninsured people leave hospitals increasingly likely to focus on profitable services,9 which surge capacity is not. As one hospital respondent explained, “There is the tension of wanting to be prepared against the competing priority of not having the budget to do so.” A recent report by congressional Democrats warned that pending federal Medicaid changes would decrease funding for teaching and public hospitals, further challenging their ability to respond to disasters.10
Although increased funding would not address every challenge—it is not feasible to stockpile staff, for example—respondents commonly reported that additional funds could help address general workforce shortages and provide more emergency response training. Moreover, federal funding for surge capacity has declined in recent years, and respondents are concerned about having the resources to maintain the plans, systems, training and supplies they have established.
Back to Top
Planning, Coordination Key
![]() ommunities are attempting to build broad surge capacity,
ranging from communication to transportation to hospital care to handling mass
fatalities. To effectively do so, respondents stressed the importance of ongoing
planning and coordination among stakeholders to determine who has resources,
who has authority and who to request help from. To that end, one of the early
benefits of federal funding after 9/11 was improved coordination among public
health agencies, fire and police departments, emergency management agencies,
and health care providers.11
ommunities are attempting to build broad surge capacity,
ranging from communication to transportation to hospital care to handling mass
fatalities. To effectively do so, respondents stressed the importance of ongoing
planning and coordination among stakeholders to determine who has resources,
who has authority and who to request help from. To that end, one of the early
benefits of federal funding after 9/11 was improved coordination among public
health agencies, fire and police departments, emergency management agencies,
and health care providers.11
Lessons from past emergencies have prompted health agencies to partner with more entities. Hurricane Katrina, for example, highlighted the need for police to provide adequate security at hospitals and other sites. State and local emergency management agencies and emergency medical services (EMS) have become more involved, particularly in transportation for workers and victims, as have morgues and mortuaries in planning for mass fatalities. Although many hospitals have long participated in collaborative community planning, some communities, such as the King County Health Care Coalition in Seattle, are pulling together broader hospital consortiums and work more closely with hospital associations. Community efforts increasingly involve community health centers (CHCs) and long-term and mental health care providers to address the distinct needs of vulnerable populations.
Organizations and communities are also creating incident command structures to enable a common and effective response within and across entities. Many communities have a unified command structure, in which the lead agency activates the emergency operations center, the central coordinating body. Fire or police might lead initially, with the public health and health care community brought in when a public health or medical response is needed. In Boston, the local public health commission leads a unified command structure, including representatives of EMS, hospitals, CHCs and the state health department. In contrast, respondents in Phoenix cited a lack of coordination among such groups as a barrier to their response plans.
Communities are developing their ability to “go it alone” for a few days after a disaster or much longer during a severe pandemic because the breadth of the event would limit outside assistance. They also are attempting to improve coordination across regional, state and federal levels to arrange for outside assistance when possible, which often requires overcoming legal and political challenges. Respondents in New Orleans and other communities noted that the lack of clear lines of communication and authority among jurisdictions hampered response to Hurricane Katrina.
Respondents extolled the virtues of frequent exercises and drills that simulate an emergency to familiarize stakeholders with the response plan and identify gaps. Hospitals conduct their own drills and exercises each year, often in concert with community-wide efforts, with some exercises focusing on a particular aspect of surge capacity. Large-scale exercises are expensive and difficult to organize since participants must also care for real patients, so a number of exercises are “tabletops,” where leaders across sectors meet to discuss response scenarios and processes. In addition, many communities use scheduled events, such as marathons, to test their plans.
Inadequate communication is a common problem identified through real emergencies and exercises. Communities have ramped up communication systems to be interoperable across various organizations, reliable so they can withstand the elements, and redundant, assuming that some systems will fail. Many communities have developed Web-based information portals at hospitals and public health and emergency management agencies and use 800 megahertz radios and ham radio networks, staffed by community volunteers, as back-up systems. Respondents, nonetheless, stressed the need for clearer communication processes, messaging and training so that all stakeholders understand the status of a situation and what to do in response. As a hospital respondent in New York City explained, “Using equipment is not that stressful, but it’s what you say, how you say it, and how you communicate it—that’s something we have virtually no training in.”
Back to Top
Stockpiling Supplies
![]() o care for many people in an emergency, states, communities and hospitals are stockpiling medical equipment and supplies. Respondents reported that federal funding often favors purchase of such items because they are more tangible and quantifiable than training. Common acquisitions include decontamination showers for use in a chemical event, the anti-viral drug Tamiflu and ventilators for pandemic flu, and cots and personal protective equipment for a host of threats. Past emergencies also have stressed the need to ensure facilities have the basics—water, food and generator fuel—to remain operational and take care of patients.
o care for many people in an emergency, states, communities and hospitals are stockpiling medical equipment and supplies. Respondents reported that federal funding often favors purchase of such items because they are more tangible and quantifiable than training. Common acquisitions include decontamination showers for use in a chemical event, the anti-viral drug Tamiflu and ventilators for pandemic flu, and cots and personal protective equipment for a host of threats. Past emergencies also have stressed the need to ensure facilities have the basics—water, food and generator fuel—to remain operational and take care of patients.
Hospitals struggle with the costs of storage, maintenance and training associated with emergency equipment and supplies. Financial pressures have required hospitals to use just-in-time inventories where they purchase only enough to meet their day-to-day needs. Federal inventory and auditing requirements, the need to rotate and replace expired drugs, and training on specialized equipment require additional staff or place additional requirements on existing staff, costs which are not often covered by federal grant funding. As one respondent bemoaned, “Everyone is big on buying the decontamination tent, buying this, buying that, and throwing money at the problem. If you can’t train people to use that ‘thing,’ it’s a big white elephant in my mind.” In response, some states and local governments have purchased standardized equipment and supplies to share or distribute among hospitals in an emergency, and some hospitals have mutual-aid agreements to share essential items. Seattle has developed a software system called KCHealthTrac that will coordinate the distribution of supplies across facilities during an emergency.
Further, respondents urged a shift in focus to equipment and supplies that can be helpful both in an emergency and on a daily basis. Easing of federal requirements could allow durable items purchased with surge capacity monies, such as wheelchairs and cots, to be used during routine crowding. Similarly, a Greenville hospital respondent praised the flexibility to purchase items with multiple uses, such as a mannequin they routinely use for training on a number of medical interventions. As the respondent noted, “Toys are nice, but you can’t buy a bunch of stuff that only gets pulled out for training and not for actual use, when you can buy stuff that will help on a day-to-day basis and improve the situation when there is a surge.”
Back to Top
Strategies to Create Space
![]() n an emergency, hospitals expect to be inundated with additional
patients, their families and friends, and others who simply seek a safe haven.
Hospitals have worked to determine how to maximize existing space, for example,
by using conference rooms and cafeterias for sleeping quarters, converting single
patient rooms into double rooms and placing patients in clinic or procedure
areas or on cots in hallways. These “alternate use” plans include determining
the types of patients best cared for in those spaces, as well as the staffing
and other resources needed. A number of communities, such as Greenville and
Miami, have plans to set up medical tents outside, although Boston does not
rely on tents because of the colder climate.
n an emergency, hospitals expect to be inundated with additional
patients, their families and friends, and others who simply seek a safe haven.
Hospitals have worked to determine how to maximize existing space, for example,
by using conference rooms and cafeterias for sleeping quarters, converting single
patient rooms into double rooms and placing patients in clinic or procedure
areas or on cots in hallways. These “alternate use” plans include determining
the types of patients best cared for in those spaces, as well as the staffing
and other resources needed. A number of communities, such as Greenville and
Miami, have plans to set up medical tents outside, although Boston does not
rely on tents because of the colder climate.
Inadequate staffing levels limit the degree to which additional spaces are useable for patient care. Many hospitals suffer from a shortage of staffed beds, which hinders their ability to take in more patients.12 In an emergency, hospitals could free up staffed beds by first discharging patients who could safely go home and canceling elective procedures. A Washington, D.C., hospital respondent pointed to their accomplishment during 9/11 of discharging almost a quarter of the hospital’s patients in four hours—consistent with the federal benchmark to free up 20 percent of hospital bed space that many communities are working toward—as reassurance that patients and physicians can rise to the occasion.
Canceling elective procedures is a short-term strategy, however, and likely not viable during a pandemic. Forgoing elective procedures also would reduce a key source of hospital revenue, and a Boston respondent indicated hospitals are reluctant to jeopardize revenues without assurances that other hospitals will do the same. Furthermore, a few respondents stressed that most elective procedures are medically necessary and could not be postponed indefinitely.
Community and regional efforts seek to create systems to identify available beds among hospitals and coordinate sending patients to a facility with space. Boston, Greenville, Seattle and Phoenix have real-time, Web-based bed tracking systems that indicate which facilities have capacity to take more patients. Although vital in an emergency, hospitals also use the systems to manage routine crowding.
Strategies to move patients among hospitals are limited to relatively contained events and when transportation is possible. For example, although hospitals in Miami routinely take in patients evacuated from the Florida Keys during moderate hurricanes, patient evacuations were more difficult during Hurricane Katrina. Enhanced use of telemedicine could help share resources when space is tight or transportation difficult: in Phoenix, telemedicine has enabled the state’s only burn center to help 10 area hospitals to each care for two to three burn patients.
Communities also are making arrangements with non-traditional facilities, such as schools, churches, hotels or convention centers, that could be used as alternate care sites in a large-scale emergency. During the 2006 windstorms in Seattle, for instance, a community college was used to house residents of a nursing home where power failed. Often, however, communities need assistance to gain the participation of such alternative facilities. Although Boston and Phoenix respondents were relatively confident in their ability to expand into non-traditional space because of their strong relationships with these facilities, Miami and New Orleans have faced resistance from facilities concerned about potential negative publicity, liability and loss of business.
Back to Top
Stretching Staff
![]() ven if additional space can be made available in an emergency,
communities are most concerned about having an adequate workforce to make such
space usable for patient care. The day-to-day shortages of key health personnel—such
as nurses, physicians, pharmacists, laboratory technicians and respiratory therapists—exacerbate
the challenge of having sufficient numbers of health workers in an emergency.
As physicians increasingly practice outside of hospitals, many emergency departments
(EDs) face significant challenges getting specialists to serve on call on a
daily basis.13 Moreover, some respondents expect approximately
40 percent of staff will not report for work during emergencies. Communities
and hospitals are pursuing a number of avenues to address these workforce limitations.
ven if additional space can be made available in an emergency,
communities are most concerned about having an adequate workforce to make such
space usable for patient care. The day-to-day shortages of key health personnel—such
as nurses, physicians, pharmacists, laboratory technicians and respiratory therapists—exacerbate
the challenge of having sufficient numbers of health workers in an emergency.
As physicians increasingly practice outside of hospitals, many emergency departments
(EDs) face significant challenges getting specialists to serve on call on a
daily basis.13 Moreover, some respondents expect approximately
40 percent of staff will not report for work during emergencies. Communities
and hospitals are pursuing a number of avenues to address these workforce limitations.
Staff-sharing arrangements. Agreements to distribute staff on the basis of need can help surge response. For example, Boston and Greenville hospitals have established memoranda of understanding to share physicians and nurses if an event affects some facilities more than others. Such agreements could be of limited value in large-scale events. As a Washington, D.C., hospital respondent lamented, “The reality is that, if it’s a regional event, everybody’s competing for the same pool of people. There are just not a lot of pharmacists, doctors or nurses.” Some respondents suggested enhanced efforts to cluster patients by needs and allocate specialists among hospitals accordingly to gain economies of scale in patient care.
Volunteers. Many communities are expanding their Medical Reserve Corps (MRC), local bodies of mostly medical professionals who agree to assist during an emergency. The national MRC includes more than 150,000 volunteers,14 with New York City’s corps the largest at approximately 7,000. Communities are at different stages of developing the Emergency System for Advance Registration of Volunteer Health Professionals (ESAR-VHP) database, a requirement by ASPR to rapidly verify volunteers’ identities and privileges to facilitate their deployment to health care facilities. In some cases, as in Hurricane Katrina, respondents reported that volunteers bring limited benefit because they need significant direction and support. Others think enhanced planning, training and more routine use of volunteers would improve their effectiveness; a Boston respondent stressed that a “just add water” system must be in place.
Worker resiliency. Rather than expecting many health care workers to come in from elsewhere, hospital and emergency managers are focusing on ways to ensure that their own staff present for work in an emergency—what one respondent described as “worker resiliency.” Hospitals are developing plans to dedicate space, food and other care for staff members’ families and pets during an emergency to enable staff to come to work. In a pandemic flu scenario, plans to provide prophylaxis to staff and their families are common. Additionally, communities with significant disaster experience, such as New Orleans and Miami, have divided staff into two teams—one team works the initial hours of an emergency, the second team replaces it—to create clear expectations and reduce fatigue. Some New York City hospitals have made participation in emergency response a condition of admitting privileges for physicians, but the strength of these arrangements has not been tested. A few respondents suggested allocating federal funding toward hazardous duty pay as an incentive to work during an emergency.
Expanding staff roles. Health organizations are trying to stretch available staff by expanding their roles in an emergency. Respondents at multiple levels of government and hospital management acknowledged that workers frequently perform outside of their normal roles during an emergency, but few have policies outlining those roles. California plans to assign state workers additional roles, based on their skills, during a disaster. New York City has conducted extensive training with hospital staff, including security guards and greeters, to triage patients for pandemic flu. Along with liability concerns, hospitals across the communities fear that expanding clinicians’ scope of care could jeopardize their accreditation and reimbursement. To some extent this is a state issue, because states determine the scope of practice for licensed health professionals.
Adapting standards of care. Hospitals and other providers would likely need to ration or reduce the level of care provided during an emergency. ASPR and the Agency for Healthcare Research and Quality have published approaches for providing the highest possible standard of care given austere conditions.15 Even so, respondents noted the need for policies to help them allocate limited staff and other resources in an emergency. Some communities, such as New York City, New Orleans and Seattle, have started initiatives to modify care protocols in an emergency, such as distribution of ventilators during a pandemic flu or the number of emergency responders or nurses attending to each patient.
Back to Top
Controlling Demand for Hospital Services
![]() reater involvement of other types of health care providers is needed to take some of the pressure off of hospitals during an emergency. Communities are trying to overcome what a Greenville respondent described as “the status quo, which has always been to go to the hospital.” Efforts to engage other providers and encourage patients to use them could also help reduce day-to-day use of the ED for non-emergent conditions.
reater involvement of other types of health care providers is needed to take some of the pressure off of hospitals during an emergency. Communities are trying to overcome what a Greenville respondent described as “the status quo, which has always been to go to the hospital.” Efforts to engage other providers and encourage patients to use them could also help reduce day-to-day use of the ED for non-emergent conditions.
Communities are increasingly looking to specialized providers—such as long-term care and mental health facilities—to remain operational during an emergency and respond to their patients’ needs. The Miami community has worked more closely with dialysis centers and other health care providers on preparedness after a hurricane caused dialysis centers to lose electricity and shut down, and dialysis patients inundated hospitals for treatment. Further, behavioral health services provide important support to families of victims and to response workers during and after an event.
Additionally, given some respondents’ estimates that many people presenting to hospitals in an emergency could be “walking wounded,” care can be provided at other sites. The Emergency Medical Treatment & Labor Act (EMTALA) has been amended to allow EDs to relocate patients for screening during a pandemic outbreak. Some local agencies are collaborating with other providers to identify screening sites to take pressure off of hospitals and assessing situations when it would be more helpful for practitioners to remain in their respective facilities to treat patients, rather than potentially volunteering at a hospital. Community health centers have been increasingly integrated into surge plans in many communities to offer primary care but gaining participation from private-practice physicians has been more difficult.
Opportunities also exist to improve public communication to educate and link people to appropriate health services to help individuals be more self sufficient and reduce their reliance on 911 systems and emergency departments. Joint information centers (JICs) allow public information officers for hospitals and local agencies to provide consistent messages to the public in an emergency, including informing the public when it is appropriate to seek care at a hospital. Also, many communities have developed public information campaigns and other educational efforts that encourage families to create their own disaster plans and self-care supply caches. Some communities have Web-based systems or other technology to help guide people to appropriate health care resources, and some respondents expressed interest in establishing staffed call centers to provide more personalized assistance.
In addition, many communities are improving communication with people with special needs, including those with mental or physical disabilities, the elderly and non-English speaking residents. Miami and New Orleans collaborate with the providers for these groups to ensure their patients can be evacuated to special-needs shelters rather than hospitals in the event of a hurricane or other disaster. Federal agencies are working to develop functional definitions for at-risk populations to help emergency planners better allocate resources according to individuals’ abilities and needs.
Back to Top
Implications
![]() ecuring adequate surge capacity at the community level is difficult and expensive. The communities in this study reported significant progress in strengthening their ability to respond to a large-scale surge in injured or ill people, although this level of readiness has required hundreds of millions of dollars and countless personnel hours over nearly a decade to achieve. Declines in federal support threaten to divert attention from the importance of surge capacity and stunt, if not undo, the capacity communities have built to respond to the next large-scale disaster. The findings of this study provide three important implications for policy makers:
ecuring adequate surge capacity at the community level is difficult and expensive. The communities in this study reported significant progress in strengthening their ability to respond to a large-scale surge in injured or ill people, although this level of readiness has required hundreds of millions of dollars and countless personnel hours over nearly a decade to achieve. Declines in federal support threaten to divert attention from the importance of surge capacity and stunt, if not undo, the capacity communities have built to respond to the next large-scale disaster. The findings of this study provide three important implications for policy makers:
First, surge capacity planning, development and deployment require broad-based support and participation and collaboration among many private and public organizations. Efforts to plan, train and exercise across sectors as diverse as health care providers, mortuaries, police, schools, transportation and businesses require resources often not included in their respective revenue streams, and additional coordination across sectors and jurisdictions.
Second, policy makers cannot ignore the tension created by a competitive health care environment in which financing arrangements do not support idle capacity. To the extent that policy makers expect surge capacity to be available, they need to assure adequate funding and guidance.
Third, until policy makers address the many health care workforce challenges confronting day-to-day service delivery, the ability to have adequate personnel for an emergency will be limited.
Communities fear that attention to surge capacity is rapidly waning. Without continued federal funding and policy attention, surge capacity developments and achievements are likely to erode.
Back to Top
Notes
Back to Top
Data Source
This study examined surge capacity in six communities from the Community Tracking Study (CTS), an ongoing study of local health care markets in 12 nationally representative metropolitan communities. Based on preliminary findings from the 2007 CTS site visits, researchers selected six communities that demonstrated a significant level of activity around surge capacity development: Boston; Greenville, S.C.; Miami; Phoenix; Orange County, Calif.; and Seattle. Interviews also were conducted with officials in New York City, Washington, D.C., and New Orleans, as well as with national leaders. Fifty-four interviews were conducted between November 2007 and January 2008 with representatives of state and local emergency management agencies and health departments, hospital emergency preparedness coordinators and other organizations working on surge capacity. A two-person research team conducted each interview, and notes were transcribed and jointly reviewed for quality and validation purposes. Interview data were coded and analyzed using Atlas.ti, a qualitative software package.
Back to Top
Funding Acknowledgement: This research was supported under a grant from a special solicitation for Public Health Systems Research through the Robert Wood Johnson Foundation’s Health Care Financing and Organization Initiative, which is administered by AcademyHealth.
ISSUE BRIEFS are published by the
Center for Studying Health System Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org