Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


Competition Revs Up the Indianapolis Health Care Market
Community Report No. 1
Winter 2003
Aaron Katz, Robert E. Hurley, Kelly Devers, Leslie Jackson Conwell, Bradley C. Strunk, Andrea Staiti, J. Lee Hargraves, Robert A. Berenson
 n September 2002, a team of researchers visited Indianapolis to study that community’s
health system, how it is changing and the effects of those changes on consumers.
The Center for Studying Health System Change (HSC), as part of the Community Tracking Study, interviewed more than 100 leaders in the health care market. Indianapolis is one of 12 communities tracked by HSC every two years through site visits and every three years through surveys. Individual community reports are published for each round of site visits. The first three site visits to Indianapolis, in 1996, 1998 and 2000, provided the background against which changes are tracked. The Indianapolis market encompasses a nine-county region that includes Boone, Hamilton, Hancock,
Hendricks, Johnson, Madison, Marion, Morgan and Shelby counties.
Once a model of genteel competition, the Indianapolis health
care market appears on the verge of becoming a battleground among providers. Physician
specialists are exercising growing leverage with the market’s four hospital systems,
seeking a share of facility fees to offset historically stagnant professional
fees. In addition, a relatively weak health plan market seems relegated to serving
as a messenger for providers seeking higher payments. Stung by rising premiums,
employers feel powerless as provider competition heats up and the economy cools
down.
Among the key market trends: n September 2002, a team of researchers visited Indianapolis to study that community’s
health system, how it is changing and the effects of those changes on consumers.
The Center for Studying Health System Change (HSC), as part of the Community Tracking Study, interviewed more than 100 leaders in the health care market. Indianapolis is one of 12 communities tracked by HSC every two years through site visits and every three years through surveys. Individual community reports are published for each round of site visits. The first three site visits to Indianapolis, in 1996, 1998 and 2000, provided the background against which changes are tracked. The Indianapolis market encompasses a nine-county region that includes Boone, Hamilton, Hancock,
Hendricks, Johnson, Madison, Marion, Morgan and Shelby counties.
Once a model of genteel competition, the Indianapolis health
care market appears on the verge of becoming a battleground among providers. Physician
specialists are exercising growing leverage with the market’s four hospital systems,
seeking a share of facility fees to offset historically stagnant professional
fees. In addition, a relatively weak health plan market seems relegated to serving
as a messenger for providers seeking higher payments. Stung by rising premiums,
employers feel powerless as provider competition heats up and the economy cools
down.
Among the key market trends:
- Single-specialty groups and hospitals have sought to bolster revenues by
developing six new specialty hospitals and expanding service areas.
- Concern is growing among providers that Anthem—long a dominant player
locally and now a national power—will flex its muscles in contract and
payment negotiations.
- The community’s health care safety net has grown stronger, thanks to state
funding and local leadership, but is threatened by state budget cuts.
Pursuit of Profits Shakes Up Provider Market
 hysician and hospital ventures are disrupting the long stable
Indianapolis market, which has been characterized by four hospital systems with
mutually exclusive geographic niches. Since the late 1990s, physician specialty
groups have grown in size and strength and now have moved aggressively to compete
for a greater share of facility fees from inpatient and outpatient services. Local
cardiovascular surgery groups initiated discussions about building heart hospitals
with MedCath, a for-profit national firm. To stave off the potential loss of physicians
and their patients, hospital systems forged partner-ships with the specialists
to consolidate or expand heart surgery programs. By late 2002, each of the four
hospital systems was building or had opened a freestanding heart facility—two
as joint ventures with physicians.
The building binge did not stop with heart surgery: hysician and hospital ventures are disrupting the long stable
Indianapolis market, which has been characterized by four hospital systems with
mutually exclusive geographic niches. Since the late 1990s, physician specialty
groups have grown in size and strength and now have moved aggressively to compete
for a greater share of facility fees from inpatient and outpatient services. Local
cardiovascular surgery groups initiated discussions about building heart hospitals
with MedCath, a for-profit national firm. To stave off the potential loss of physicians
and their patients, hospital systems forged partner-ships with the specialists
to consolidate or expand heart surgery programs. By late 2002, each of the four
hospital systems was building or had opened a freestanding heart facility—two
as joint ventures with physicians.
The building binge did not stop with heart surgery:
- Orthopedics Indianapolis, a large single-specialty
group, announced plans to build
its own orthopedic hospital to supplement
its existing freestanding surgery center.
- St. Vincent’s Hospital and Health System
opened a new children’s hospital to compete
with Clarian’s Riley Children’s Hospital
(affiliated with Indiana University), for
many years the only children’s hospital in
the market.
- Physician specialty groups were building
outpatient facilities alone or in conjunction
with hospitals as well as incorporating
more diagnostic and laboratory testing
into their own practices.
And the spree may not be over. Some market observers expressed concern that
oncologists will initiate discussions with a for-profit national company, spurring hospitals
to build additional outpatient cancer facilities that physicians would partly own.
Competition among hospitals also has been heating up and may be breaking down
the market’s exclusive geographic spheres of influence. Several hospital systems
announced plans to build new hospitals or make significant renovations to existing
facilities in areas where competing systems are located. Some of the construction
is designed to move services of flagship hospitals into more lucrative and faster-growing
areas, particularly outside the city of Indianapolis. Competition among hospitals
also has been spurred by ongoing friction between physicians from Indiana University
and Methodist Hospital, which merged in 1997 to form Clarian Health System. Many
physicians affiliated with Methodist have moved to other hospitals, fueling growth
in programs at these competitors and potentially undermining Clarian’s dominant
market position.
The newly competitive Indianapolis market is likely to have significant effects on consumers. New facilities and services could lead to greater access to providers (at least for privately insured patients), lower costs and higher clinical quality as providers manage care better and compete for patients. However, providers have little incentive to focus on care management in a market dominated by preferred provider organizations (PPOs) that pay discounted fee-for-service or case rates and that do not differentiate among providers based on performance. Indeed, improving clinical quality did not appear to be a driving force for new facilities or services. Given these market conditions, provider competition could, alternatively, result in higher use rates and costs. Competition over specialty services also could lure profitable services away from general hospitals, draining revenues needed to cross-subsidize less profitable services, including care for the uninsured.
The escalating competitive behavior observed among providers suggests that Indianapolis is a health care market in motion without private market or public
regulatory brakes. In some parts of the country, pressure from purchasers, health plan negotiators or state regulators might be expected to slow down or divert bricks-and-
mortar competition. However, the 2002 Indianapolis market revealed none of
these forces: employers have little leverage with health care providers; health plans
seem resigned to passing on providers’ demands for higher payments; and state
policy makers have few tools to influence expansion decisions, having long ago
repealed certificate-of-need laws.
Back to Top
Purchasers Face Rising Premiums, Weak Economy
 mployers wield little power over the Indianapolis health care
market and have limited options in the face of a weak economy and steep health
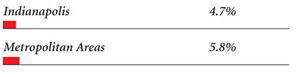
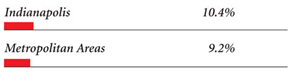
benefit cost increases. Insurance premiums began to rise in double digits in the
late 1990s. Unemployment was low then, about 2.6 percent, so businesses generally
absorbed these costs—rather than shift costs or cut benefits—to compete
for workers. However, unemployment in Indianapolis jumped to 4.6 percent in 2002,
a large increase though still below the national average of 5.8 percent. The higher
unemployment rate makes it easier for employers to increase employee cost sharing
or to explore more novel benefit strategies. In fact, faced with premium increases
of about 15 percent in 2002 and another 20 percent in 2003, employers in Indianapolis
are increasing deductibles and copayments, especially for prescription drug benefits,
and exploring consumer-driven health plans.
However, beyond cost-sharing changes, individual employers have not harnessed
their purchasing power to make demands of providers or plans. Public employers
have not been aggressive purchasers, while large private firms often have relationships
with health care organizations—such as serving on their boards—that
may blunt their ability to put pressure on the delivery system. For example, its
belief that improved quality will lower costs has spurred Eli Lilly over the years
to lead other large employers in collaborative efforts to improve the health care
delivery system. However, plan and provider respondents noted that Lilly must
proceed cautiously to avoid angering or alienating providers that purchase the
drug manufacturer’s products.
Although purchasers are not a significant force in Indianapolis, it is not for lack of trying. Since 1996, four different employer organizations have attempted to improve the health care delivery system. None of these organizations has had a sustained impact, in part because employers have had difficulties deciding among themselves what the goal of their efforts should be.
To make things worse, the weak economy has led to a decline in the number of corporate headquarters in Indianapolis: several large employers left the market, including the USA Group and Ameritech; the banking and insurance industries have consolidated; and Conseco, a financial services company in Carmel, declared bankruptcy at the end of 2002. The loss of headquarters may make it harder to develop effective coalitions that can shape the Indianapolis health care market. In all, this history led to a marked change in employer attitudes between 2000 and 2002, from being excited about the potential of their planned efforts to being more subdued and less optimistic about their ability to control costs.
Yet, employers are attempting once again to harness their power through the new Employers’ Forum, which aims to manage costs and promote employees’ involvement in health care decisions while also creating an environment that is responsive to the disparate needs of employers, providers and plans. What specific actions the forum will take was unclear in late 2002, and sustained buy-in from the employer community is uncertain. mployers wield little power over the Indianapolis health care
market and have limited options in the face of a weak economy and steep health
benefit cost increases. Insurance premiums began to rise in double digits in the
late 1990s. Unemployment was low then, about 2.6 percent, so businesses generally
absorbed these costs—rather than shift costs or cut benefits—to compete
for workers. However, unemployment in Indianapolis jumped to 4.6 percent in 2002,
a large increase though still below the national average of 5.8 percent. The higher
unemployment rate makes it easier for employers to increase employee cost sharing
or to explore more novel benefit strategies. In fact, faced with premium increases
of about 15 percent in 2002 and another 20 percent in 2003, employers in Indianapolis
are increasing deductibles and copayments, especially for prescription drug benefits,
and exploring consumer-driven health plans.
However, beyond cost-sharing changes, individual employers have not harnessed
their purchasing power to make demands of providers or plans. Public employers
have not been aggressive purchasers, while large private firms often have relationships
with health care organizations—such as serving on their boards—that
may blunt their ability to put pressure on the delivery system. For example, its
belief that improved quality will lower costs has spurred Eli Lilly over the years
to lead other large employers in collaborative efforts to improve the health care
delivery system. However, plan and provider respondents noted that Lilly must
proceed cautiously to avoid angering or alienating providers that purchase the
drug manufacturer’s products.
Although purchasers are not a significant force in Indianapolis, it is not for lack of trying. Since 1996, four different employer organizations have attempted to improve the health care delivery system. None of these organizations has had a sustained impact, in part because employers have had difficulties deciding among themselves what the goal of their efforts should be.
To make things worse, the weak economy has led to a decline in the number of corporate headquarters in Indianapolis: several large employers left the market, including the USA Group and Ameritech; the banking and insurance industries have consolidated; and Conseco, a financial services company in Carmel, declared bankruptcy at the end of 2002. The loss of headquarters may make it harder to develop effective coalitions that can shape the Indianapolis health care market. In all, this history led to a marked change in employer attitudes between 2000 and 2002, from being excited about the potential of their planned efforts to being more subdued and less optimistic about their ability to control costs.
Yet, employers are attempting once again to harness their power through the new Employers’ Forum, which aims to manage costs and promote employees’ involvement in health care decisions while also creating an environment that is responsive to the disparate needs of employers, providers and plans. What specific actions the forum will take was unclear in late 2002, and sustained buy-in from the employer community is uncertain.
Back to Top
Weak Health Plan Market Belies Anthem’s Potential Power
 ost health plans do not exercise much leverage with providers or strong managed care strategies, and observers expect little change in the near term, despite steeply rising premiums. As providers vie for new sources of revenue, they are pressuring health plans as well to increase payment rates to meet current and future financial needs, including the estimated $500 million in construction costs for new heart hospitals and other programs. Without employer pressure to counter these demands, most plans have found it difficult to resist hospitals’ and physicians’ push for higher payments. Instead, they increased beneficiary cost sharing to offset the impact of premium increases on employers.
Plans also are exploring new types of products to promote consumer cost-consciousness, such as high-deductible plans that require even greater levels of cost sharing and personal spending account-based
models. In addition, plans are evaluating tiered provider networks that would require consumers to pay more out-of- pocket to see higher-cost providers in the plan’s network. However, demand for broad, undifferentiated provider networks and resistance from hospitals may make such products unlikely in the short run.
Meanwhile, interest in health maintenance organizations (HMOs), never strong in
Indianapolis, has continued to decline, another indication of the deterioration
of health insurance products that could moderate prices in the market. Maxicare
declared bankruptcy in 2000 after a period of decline; Aetna aborted development
of its HMO in 2001; and Anthem’s HMO enrollment continues to shrink. As a result,
the only major HMOs available are those sponsored by the provider systems themselves.
Although these plans’ networks include nonowner hospitals, it is unlikely that
they have the same drive to moderate provider payment rates as independently owned
health plans. The financial well-being of HMOs has been threatened further by
a crisis in the state’s high-risk pool (see box on page 5).
As Indianapolis continues its long-standing preference for PPOs, Indianapolis-based Anthem Blue Cross Blue Shield dominates the health plan market. Anthem maintains a large share of the market’s sizeable self-funded PPO business and accounts for the largest segment of the fully insured market, competing primarily with plans owned by the local provider systems.
Anthem’s local market presence has not changed appreciably, but its growing national
presence has heightened concern about the plan’s potential power in Indianapolis.
Anthem completed its con-version from a mutual insurance company to a publicly
traded firm in 2001 and became the fifth-largest health insurer in the country
by acquiring Blue Cross and Blue Shield plans in eight other states. The conversion
has generated some backlash among physicians who intensified com-plaints about
Anthem’s business practices, alleging down-coding—reclassifying claims to
codes with lower payment levels—and slow payment. Hospitals, too, have become
more assertive with Anthem. In 2002, St. Francis Hospital announced plans to terminate
its contract with Anthem over payment rates and contract terms, but the parties
later reached an agreement that includes quality-linked bonuses. To date, Anthem’s
potential power appears to be in check. However, if the plan becomes more aggressive
in its home market, pressure on provider payments could increase. ost health plans do not exercise much leverage with providers or strong managed care strategies, and observers expect little change in the near term, despite steeply rising premiums. As providers vie for new sources of revenue, they are pressuring health plans as well to increase payment rates to meet current and future financial needs, including the estimated $500 million in construction costs for new heart hospitals and other programs. Without employer pressure to counter these demands, most plans have found it difficult to resist hospitals’ and physicians’ push for higher payments. Instead, they increased beneficiary cost sharing to offset the impact of premium increases on employers.
Plans also are exploring new types of products to promote consumer cost-consciousness, such as high-deductible plans that require even greater levels of cost sharing and personal spending account-based
models. In addition, plans are evaluating tiered provider networks that would require consumers to pay more out-of- pocket to see higher-cost providers in the plan’s network. However, demand for broad, undifferentiated provider networks and resistance from hospitals may make such products unlikely in the short run.
Meanwhile, interest in health maintenance organizations (HMOs), never strong in
Indianapolis, has continued to decline, another indication of the deterioration
of health insurance products that could moderate prices in the market. Maxicare
declared bankruptcy in 2000 after a period of decline; Aetna aborted development
of its HMO in 2001; and Anthem’s HMO enrollment continues to shrink. As a result,
the only major HMOs available are those sponsored by the provider systems themselves.
Although these plans’ networks include nonowner hospitals, it is unlikely that
they have the same drive to moderate provider payment rates as independently owned
health plans. The financial well-being of HMOs has been threatened further by
a crisis in the state’s high-risk pool (see box on page 5).
As Indianapolis continues its long-standing preference for PPOs, Indianapolis-based Anthem Blue Cross Blue Shield dominates the health plan market. Anthem maintains a large share of the market’s sizeable self-funded PPO business and accounts for the largest segment of the fully insured market, competing primarily with plans owned by the local provider systems.
Anthem’s local market presence has not changed appreciably, but its growing national
presence has heightened concern about the plan’s potential power in Indianapolis.
Anthem completed its con-version from a mutual insurance company to a publicly
traded firm in 2001 and became the fifth-largest health insurer in the country
by acquiring Blue Cross and Blue Shield plans in eight other states. The conversion
has generated some backlash among physicians who intensified com-plaints about
Anthem’s business practices, alleging down-coding—reclassifying claims to
codes with lower payment levels—and slow payment. Hospitals, too, have become
more assertive with Anthem. In 2002, St. Francis Hospital announced plans to terminate
its contract with Anthem over payment rates and contract terms, but the parties
later reached an agreement that includes quality-linked bonuses. To date, Anthem’s
potential power appears to be in check. However, if the plan becomes more aggressive
in its home market, pressure on provider payments could increase.
Back to Top
Safety Net, Public Health Gains May be Lost as Budget Threat Looms
 ven as provider competition sweeps through the market, Indianapolis’
safety net providers and public agencies have been a model of cooperation. As
was the case two years ago, leadership by the Health and Hospital Corporation
(HHC) of Marion County—including Wishard Health Services (the public Wishard
Hospital and six community health centers) and the Marion County Health Department—was
instrumental in these new cooperative efforts that have helped to strengthen the
safety net.
In 2000, safety net providers in Indianapolis anticipated that their capacity to serve low-income people would greatly expand soon due to public program expansions and the state’s decision to dedicate its tobacco settlement funds to health care. By 2002, this expectation had been well met. As a result of aggressive outreach and enrollment activities, the state’s Medicaid managed care program, Hoosier Healthwise, grew 12 percent in Marion County, from approximately 74,750 enrollees in June 2001 to 83,600 in June 2002. Moreover, the state mandated managed care for most Medicaid beneficiaries in Marion County, the first of five Indiana counties, beginning in April 2002, and HMO enrollment now exceeds 100,000. This enrollment growth meant safety net providers are getting paid
for care they previously provided for free. The state also awarded $31 million in tobacco settlement grants in that program’s first year, which both Wishard Health Services and the HealthNet clinic system
used to expand and modernize existing facilities and to build new ones.
Enrollment in Wishard Advantage—an innovative managed care program for uninsured
people operated by Wishard Health Services—grew by 50 percent in the first
10 months of 2002, expanding from 20,000 to 30,000 participants. The growth was
due to the economic downturn and the successful two-year effort to enlist participation
of all community health centers in Marion County. A federal grant to help integrate
systems of care for the uninsured bolstered this alliance further by developing
a common copayment policy across all of these safety net providers and making
available a prescription drug assistance program to all patients. Wishard also
used the grant to develop an electronic application system that will help enrollment
in Hoosier Healthwise and Wishard Advantage. These initiatives are widely seen
as improving provider bottom lines and stretching limited resources and capacities
as much as possible.
Adding to the sense of well-being in the public sector, Indianapolis-area leaders
have made substantial progress in preparing
for possible terrorist attacks, according to
local observers. Led by Indianapolis Mayor
Bart Peterson and the local health department,
these efforts reveal a high degree of
cooperation among local public agencies
and health care entities that are competing
in other arenas. Indianapolis’ readiness may
have been helped by the city’s earlier emergency
preparedness for such large events as
the Indianapolis 500 and an anthrax scare
before Sept. 11, 2001.
Despite this cooperation and progress, state budget difficulties now threaten safety net providers and access to care for low-income residents. The state ended fiscal year 2002 with the smallest reserve since 1993, having collected $300 million less in taxes than expected, and Medicaid spending was exceeding available revenue by about $250 million. On July 1, 2002, the state eliminated continuous eligibility for Medicaid; beneficiaries now must be recertified each time their financial status changes. The state has cut Medicaid
hospital payment rates by 5 percent in each of the last two years, pharmacy payments by $37 million and nursing home spending by $108 million. Some fear the lingering recession will lead lawmakers to enact
more provider cuts, limit certain Medicaid benefits, call off the aggressive outreach efforts that expanded coverage to many of the uninsured and/or use tobacco settlement funds to shore up the overall state budget
rather than specifically for health programs. ven as provider competition sweeps through the market, Indianapolis’
safety net providers and public agencies have been a model of cooperation. As
was the case two years ago, leadership by the Health and Hospital Corporation
(HHC) of Marion County—including Wishard Health Services (the public Wishard
Hospital and six community health centers) and the Marion County Health Department—was
instrumental in these new cooperative efforts that have helped to strengthen the
safety net.
In 2000, safety net providers in Indianapolis anticipated that their capacity to serve low-income people would greatly expand soon due to public program expansions and the state’s decision to dedicate its tobacco settlement funds to health care. By 2002, this expectation had been well met. As a result of aggressive outreach and enrollment activities, the state’s Medicaid managed care program, Hoosier Healthwise, grew 12 percent in Marion County, from approximately 74,750 enrollees in June 2001 to 83,600 in June 2002. Moreover, the state mandated managed care for most Medicaid beneficiaries in Marion County, the first of five Indiana counties, beginning in April 2002, and HMO enrollment now exceeds 100,000. This enrollment growth meant safety net providers are getting paid
for care they previously provided for free. The state also awarded $31 million in tobacco settlement grants in that program’s first year, which both Wishard Health Services and the HealthNet clinic system
used to expand and modernize existing facilities and to build new ones.
Enrollment in Wishard Advantage—an innovative managed care program for uninsured
people operated by Wishard Health Services—grew by 50 percent in the first
10 months of 2002, expanding from 20,000 to 30,000 participants. The growth was
due to the economic downturn and the successful two-year effort to enlist participation
of all community health centers in Marion County. A federal grant to help integrate
systems of care for the uninsured bolstered this alliance further by developing
a common copayment policy across all of these safety net providers and making
available a prescription drug assistance program to all patients. Wishard also
used the grant to develop an electronic application system that will help enrollment
in Hoosier Healthwise and Wishard Advantage. These initiatives are widely seen
as improving provider bottom lines and stretching limited resources and capacities
as much as possible.
Adding to the sense of well-being in the public sector, Indianapolis-area leaders
have made substantial progress in preparing
for possible terrorist attacks, according to
local observers. Led by Indianapolis Mayor
Bart Peterson and the local health department,
these efforts reveal a high degree of
cooperation among local public agencies
and health care entities that are competing
in other arenas. Indianapolis’ readiness may
have been helped by the city’s earlier emergency
preparedness for such large events as
the Indianapolis 500 and an anthrax scare
before Sept. 11, 2001.
Despite this cooperation and progress, state budget difficulties now threaten safety net providers and access to care for low-income residents. The state ended fiscal year 2002 with the smallest reserve since 1993, having collected $300 million less in taxes than expected, and Medicaid spending was exceeding available revenue by about $250 million. On July 1, 2002, the state eliminated continuous eligibility for Medicaid; beneficiaries now must be recertified each time their financial status changes. The state has cut Medicaid
hospital payment rates by 5 percent in each of the last two years, pharmacy payments by $37 million and nursing home spending by $108 million. Some fear the lingering recession will lead lawmakers to enact
more provider cuts, limit certain Medicaid benefits, call off the aggressive outreach efforts that expanded coverage to many of the uninsured and/or use tobacco settlement funds to shore up the overall state budget
rather than specifically for health programs.
Back to Top
The Risky Business of High-Risk Pools
 he Indiana Comprehensive Health Insurance Association (ICHIA)—Indiana’s
state-run high-risk pool—faced a financing crisis when assessments to cover
program costs mushroomed 77 percent between 2000 and 2002. State-run high-risk
pools have been created to provide access to health insurance for people who are
medically uninsurable. Generally, people pay premiums that are pegged to some
percentage above private market rates, and costs that exceed premium income are
covered by assessments against health plans. These insurance programs often struggle
financially, because costs grow faster than collected premiums.
This fate befell ICHIA when, after steady growth since 1992, costs skyrocketed
after the state used federal grant funds to enroll people with HIV/AIDS. Health
plan assessments reached about $80 million, causing financial stress for many
local plans. Part of the problem stemmed from the fact that ICHIA assessments
were based on a health plan’s share of premium revenues in the market, which applies
only to fully insured product offerings and ignores the large amount of revenue
in the self-funded market. As a result, plans whose business was primarily in
fully insured products—namely HMOs—shouldered a disproportionately
large share of the assessment burden.
Three HMOs sued the state over the pool’s funding method, and, in late 2002, the
ICHIA board revised the method to apportion assessments based on an insurer’s
share of covered lives rather than on premium revenue. This change is expected
to reduce the overall burden on insured HMOs and increase assessments paid by
stop-loss carriers, which protect self-insured employers against very large (catastrophic)
claims. However, the steep growth in ICHIA assessments reveals how fragile the
financing of state high-risk pools—and the economic well-being of the health
plans they rely on—can be. he Indiana Comprehensive Health Insurance Association (ICHIA)—Indiana’s
state-run high-risk pool—faced a financing crisis when assessments to cover
program costs mushroomed 77 percent between 2000 and 2002. State-run high-risk
pools have been created to provide access to health insurance for people who are
medically uninsurable. Generally, people pay premiums that are pegged to some
percentage above private market rates, and costs that exceed premium income are
covered by assessments against health plans. These insurance programs often struggle
financially, because costs grow faster than collected premiums.
This fate befell ICHIA when, after steady growth since 1992, costs skyrocketed
after the state used federal grant funds to enroll people with HIV/AIDS. Health
plan assessments reached about $80 million, causing financial stress for many
local plans. Part of the problem stemmed from the fact that ICHIA assessments
were based on a health plan’s share of premium revenues in the market, which applies
only to fully insured product offerings and ignores the large amount of revenue
in the self-funded market. As a result, plans whose business was primarily in
fully insured products—namely HMOs—shouldered a disproportionately
large share of the assessment burden.
Three HMOs sued the state over the pool’s funding method, and, in late 2002, the
ICHIA board revised the method to apportion assessments based on an insurer’s
share of covered lives rather than on premium revenue. This change is expected
to reduce the overall burden on insured HMOs and increase assessments paid by
stop-loss carriers, which protect self-insured employers against very large (catastrophic)
claims. However, the steep growth in ICHIA assessments reveals how fragile the
financing of state high-risk pools—and the economic well-being of the health
plans they rely on—can be.
Back to Top
Issues to Track
 he past two years have seen Indianapolis transformed from a stable, almost predictable market to a swirl of new construction and hotly contested service areas. This dramatic shift has been sparked by the efforts of
single-specialty medical groups to secure a larger portion of hospitals’ business and by hospital strategies to carve out new market niches. Moreover, providers of all types are demanding higher payments, ostensibly to recoup after years of stagnation. With health plan, employer and public policy sectors seemingly powerless to stop the concomitant surge in costs, consumers are absorbing higher cost sharing in the midst of a weak economy.
As the new competitive market unfolds,
these issues will be important to track: he past two years have seen Indianapolis transformed from a stable, almost predictable market to a swirl of new construction and hotly contested service areas. This dramatic shift has been sparked by the efforts of
single-specialty medical groups to secure a larger portion of hospitals’ business and by hospital strategies to carve out new market niches. Moreover, providers of all types are demanding higher payments, ostensibly to recoup after years of stagnation. With health plan, employer and public policy sectors seemingly powerless to stop the concomitant surge in costs, consumers are absorbing higher cost sharing in the midst of a weak economy.
As the new competitive market unfolds,
these issues will be important to track:
- How will the new specialty facilities affect
the cost, quality and availability of health
care in Indianapolis? Will they draw
profitable business away from general
community hospitals, thus hampering
their ability to provide unprofitable
services and charity care?
- How will state budget difficulties affect
the recent progress and growth in public
insurance programs and continuing
support for the safety net? Will low-income
residents be left with less access
to needed care?
- Can health plans and employers find the
market muscle to control spending and
premium growth? If not, how will higher
cost sharing affect consumers?
- Will the newly formed Employers’ Forum have any greater success than similar
past efforts in influencing provider and plan performance in the Indianapolis
marketplace?
Back to Top
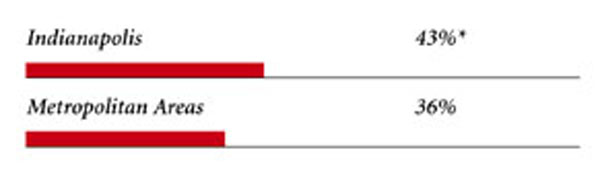
Indianapolis Consumers’ Access to Care, 2000
Indianapolis compared to metropolitan areas with over 200.000 population
| Unmet Need |
| PERSONS WHO DID NOT GET NEEDED MEDICAL CARE DURING THE LAST 12 MONTHS |
|
| Delayed Care |
| PERSONS WHO DELAYED GETTING NEEDED MEDICAL CARE DURING THE LAST 12 MONTHS
|
|
| Out-of-Pocket Costs |
| PRIVATELY INSURED PEOPLE IN FAMILIES WITH ANNUAL OUT-OF-POCKET
COSTS OF $500 OR MORE |
|
| Access to Physicians |
| PHYSICIANS WILLING TO ACCEPT ALL NEW PATIENTS WITH PRIVATE
INSURANCE |
|
| PHYSICIANS WILLING TO ACCEPT ALL NEW MEDICARE PATIENTS |
|
| PHYSICIANS WILLING TO ACCEPT ALL NEW MEDICAID PATIENTS |
|
| PHYSICIANS PROVIDING CHARITY CARE |
|
* Site value is significantly different from the mean for large metropolitan
areas over 200,000 population at p<.05.
Source: HSC Community Tracking Study Household and
Physician Surveys, 2000-01
Note: If a person reported both
an unmet need and delayed care, that person is counted as having an unmet
need only. Based on follow-up questions asking for reasons for unmet needs
or delayed care, data include only responses where at least one of the reasons
was related to the health care system. Responses related only to personal
reasons were not considered as unmet need or delayed care. |
Back to Top
Background and Observations
| Indianapolis Demographics |
| Indianapolis |
Metropolitan areas 200,000+ population |
Population1
1,620,373 |
| Persons Age 65 or Older2 |
| 11% |
11% |
| Median Family Income3 |
| $30,745 |
$31,883 |
| Unemployment Rate3 |
| 4.5% |
5.8% |
| Persons Living in Poverty2 |
| 8% |
12% |
| Persons Without Health Insurance2
|
| 12% |
13% |
| Age-Adjusted Mortality Rate per 1,000 Population4
|
| 9.8 |
8.8* |
* National average.
Sources:
1. U.S. Census Bureau, County Population Estimates, July 1, 2001
2. HSC Community Tracking Study Household Survey, 2000-01
3. Bureau of Labor Statistics, 2002 (site estimate calculated by taking
the average of monthly unemployment rates, January-December 2002)
4. Centers for Disease Control and Prevention, 1999 |
| Health Care Utilization |
| Indianapolis |
Metropolitan areas above 200,000 population |
| Adjusted Inpatient Admissions per 1,000 Population 1 |
| 225 |
180 |
| Persons with Any Emergency Room Visit in Past Year 2
|
| 20% |
19% |
| Persons with Any Doctor Visit in Past Year 2 |
| 79% |
78% |
| Average Number of Surgeries in Past Year per 100 Persons 2 |
| 18 |
17 |
Sources:
1. American Hospital Association, 2000
2. HSC Community Tracking Study Household Survey, 2000-01 |
| Health System Characteristics |
| Indianapolis |
Metropolitan areas 200,000+ population |
| Staffed Hospital Beds per 1,000 Population1
|
| 3.0 |
2.5 |
| Physicians per 1,000 Population2
|
| 2.0 |
1.9 |
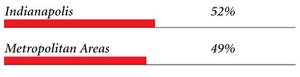
| HMO Penetration, 19993 |
| 23% |
38% |
| HMO Penetration, 20014 |
| 21% |
37% |
| Medicare-Adjusted Average per Capita Cost
(AAPCO) Rate, 20023 |
| $553 |
$575 |
Sources:
1. American Hospital Association, 2000
2. Area Resource File, 2002 (includes nonfederal, patient care physicians, except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge, 10.1
4. InterStudy Competitive Edge, 11.2
5. Centers for Medicare and Medicaid Services. Site estimate is payment
rate for largest county in site; national estimate is national per capita
spending on Medicare enrollees in Coordinated Care Plans in December 2002.
|
Back to Top

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. HSC conducts surveys in all 60 communities every
three years and site visits in 12 communities every two years. This Community
Report series documents the findings from the fourth round of site visits. Analyses
based on site visit and survey data from the Community Tracking Study are published
by HSC in Issue Briefs, Tracking Reports, Data Bulletins and peer-reviewed journals.
These publications are available at www.hschange.org.
Authors of the Indianapolis Community Report:
Aaron Katz, University of Washington; Robert E. Hurley, Virginia Commonwealth
University;
Kelly J. Devers, HSC; Leslie A. Conwell, HSC; Bradley C. Strunk, HSC; Andrea
B. Staiti, HSC;
J. Lee Hargraves, HSC; Robert A. Berenson, AcademyHealth
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Richard Sorian
Editor: The Stein Group
For additional copies or to be added to the mailing list, contact HSC at:
600 Maryland Avenue SW, Suite 550, Washington, DC 20024-2512
Tel: (202) 554-7549 (for publication information)
Tel: (202) 484-5261 (for general HSC information)
Fax: (202) 484-9258
www.hschange.org
|