Insurance Coverage & Costs
Access to Care
Uninsured and Low-Income
Racial/Ethnic Disparities
Safety Net Providers
Community Health Centers
Hospitals
Physicians
Insured People
Quality & Care Delivery
Health Care Markets
Insurance Coverage & Costs
Access to Care
Uninsured and Low-Income
Racial/Ethnic Disparities
Safety Net Providers
Community Health Centers
Hospitals
Physicians
Insured People
Quality & Care Delivery
Health Care Markets
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


Rapid Population Growth Attracts National Firms
Phoenix, Arizona
Community Report No. 04
Winter 2001
Debra A. Draper, Linda R. Brewster, Lawrence D. Brown, Carolyn A. Watts, Laurie E. Felland, Jon B. Christianson, Jeffrey Stoddard, Michael H. Park
 n September 2000, a team of
researchers visited Phoenix, Ariz., to
study that community’s health system,
how it is changing and the effects
of those changes on consumers. The
Center for Studying Health System
Change (HSC), as part of the
Community Tracking Study, interviewed
more than 85 leaders in the
health care market. Phoenix is one of
12 communities tracked by HSC
every two years through site visits and
surveys. Individual community
reports are published for each round
of site visits. The first two site visits to
Phoenix, in 1996 and 1998, provided
baseline and initial trend information
against which changes are
tracked. The Phoenix market encompasses
Maricopa and Pinal counties. n September 2000, a team of
researchers visited Phoenix, Ariz., to
study that community’s health system,
how it is changing and the effects
of those changes on consumers. The
Center for Studying Health System
Change (HSC), as part of the
Community Tracking Study, interviewed
more than 85 leaders in the
health care market. Phoenix is one of
12 communities tracked by HSC
every two years through site visits and
surveys. Individual community
reports are published for each round
of site visits. The first two site visits to
Phoenix, in 1996 and 1998, provided
baseline and initial trend information
against which changes are
tracked. The Phoenix market encompasses
Maricopa and Pinal counties.
With the addition of 100,000 people a year, Phoenix
continues to grow rapidly, making its health care market
attractive to national firms. A series of hospital acquisitions
since 1998 has left these firms in control of the
majority of the area’s hospital capacity. National firms are
also dominant in the health plan market, although a new
focus on profitability is leading some to eliminate unprofitable
lines of business, including Medicare+Choice. A
national hospital management company is credited with
helping to stabilize the community’s major safety-net
provider, but concerns remain about the area’s capacity to
care for the uninsured.
Against this backdrop, key developments in Phoenix
since 1998 include:
- Hospitals began to increase their leverage with health
plans, but financial pressures mounted as some physicians
shifted focus from hospitals to independent
specialty facilities.
- Changes to plans’ Medicare+Choice products have left
seniors with fewer choices and higher costs.
- Arizona citizens used ballot initiatives to secure funding
to care for the uninsured.
Hospital Systems Consolidate and Gain Leverage
 ooming population growth has led many Phoenix hospitals to pursue affiliations
with national systems to obtain capital necessary to respond to increasing demand.
As a result of acquisitions, the Phoenix market has 10 hospital systems (excluding
specialty hospitals)- down from 13 systems two years ago. The most significant
acquisition was a merger between Samaritan Health System, the area’s largest provider
system, and the national Lutheran Health Network to form BannerHealth Arizona-
a five-hospital system that accounts for the largest share of hospital capacity
in Phoenix.
Other national firms active in the
market are Catholic Healthcare West,
Vanguard Health Systems, Iasis Healthcare,
Triad Hospitals and Quorum Health
Resources. National firms now control 70
percent of the Phoenix community’s
hospital capacity, a figure that may soon
increase if Vanguard acquires PMH
Resources, owner of Phoenix Memorial
Hospital, as some observers speculate.
Several hospitals have turned to
their new partners for capital to fund
facility upgrades and new competitive
ventures. BannerHealth Arizona, for
example, has initiated an $88 million
project to expand capacity at Desert
Samaritan and Thunderbird Samaritan
hospitals, and it recently completed construction
of a 60-bed heart hospital on
the campus of Mesa Lutheran Hospital
in a joint venture with local cardiologists.
Likewise, Catholic Healthcare West is
undertaking $21 million in renovations
to expand capacity at Chandler Regional
Hospital in the East Valley and plans to
expand pediatric and neonatology services
at St. Joseph’s Hospital downtown.
However, the shortage of nurses and other
health care professionals may limit hospitals’
ability to bring new capacity on line.
Since 1998, Phoenix hospitals have
made strategic moves to gain footholds in
specific areas of the geographically broad
market to ensure their indispensability to
health plan networks. As one hospital
executive put it, "Geography is destiny"
in the Phoenix market. Most hospital systems
have focused their strategic efforts
on securing strongholds in key geographic
submarkets. Catholic Healthcare West, for
example, strengthened its market position
with the acquisition of Chandler Regional
Hospital, which gave it a foothold in the
rapidly growing East Valley. Newly consolidated
BannerHealth Arizona has a
strong market position because it offers
the broadest geographic coverage in
the market.
Health plans report that hospitals’
virtual monopolies in certain geographic
areas give hospitals a significant advantage
in negotiations, resulting in more favorable
contract terms and higher payment
rates for hospitals. In addition, plans contend
that BannerHealth Arizona has
begun to leverage its strong market position
and name-brand recognition to
secure higher payment rates and better
contract terms, limiting health plans’
ability to hold down costs. ooming population growth has led many Phoenix hospitals to pursue affiliations
with national systems to obtain capital necessary to respond to increasing demand.
As a result of acquisitions, the Phoenix market has 10 hospital systems (excluding
specialty hospitals)- down from 13 systems two years ago. The most significant
acquisition was a merger between Samaritan Health System, the area’s largest provider
system, and the national Lutheran Health Network to form BannerHealth Arizona-
a five-hospital system that accounts for the largest share of hospital capacity
in Phoenix.
Other national firms active in the
market are Catholic Healthcare West,
Vanguard Health Systems, Iasis Healthcare,
Triad Hospitals and Quorum Health
Resources. National firms now control 70
percent of the Phoenix community’s
hospital capacity, a figure that may soon
increase if Vanguard acquires PMH
Resources, owner of Phoenix Memorial
Hospital, as some observers speculate.
Several hospitals have turned to
their new partners for capital to fund
facility upgrades and new competitive
ventures. BannerHealth Arizona, for
example, has initiated an $88 million
project to expand capacity at Desert
Samaritan and Thunderbird Samaritan
hospitals, and it recently completed construction
of a 60-bed heart hospital on
the campus of Mesa Lutheran Hospital
in a joint venture with local cardiologists.
Likewise, Catholic Healthcare West is
undertaking $21 million in renovations
to expand capacity at Chandler Regional
Hospital in the East Valley and plans to
expand pediatric and neonatology services
at St. Joseph’s Hospital downtown.
However, the shortage of nurses and other
health care professionals may limit hospitals’
ability to bring new capacity on line.
Since 1998, Phoenix hospitals have
made strategic moves to gain footholds in
specific areas of the geographically broad
market to ensure their indispensability to
health plan networks. As one hospital
executive put it, "Geography is destiny"
in the Phoenix market. Most hospital systems
have focused their strategic efforts
on securing strongholds in key geographic
submarkets. Catholic Healthcare West, for
example, strengthened its market position
with the acquisition of Chandler Regional
Hospital, which gave it a foothold in the
rapidly growing East Valley. Newly consolidated
BannerHealth Arizona has a
strong market position because it offers
the broadest geographic coverage in
the market.
Health plans report that hospitals’
virtual monopolies in certain geographic
areas give hospitals a significant advantage
in negotiations, resulting in more favorable
contract terms and higher payment
rates for hospitals. In addition, plans contend
that BannerHealth Arizona has
begun to leverage its strong market position
and name-brand recognition to
secure higher payment rates and better
contract terms, limiting health plans’
ability to hold down costs.
Physicians Shift Focus to Specialty Facilities
 hysicians’ discontent with the local
health care system has reached new
heights over the past two years, and
physicians are aggressively pursuing
strategies to improve their financial
situations. Perhaps most significant,
some specialists have cut back on their
affiliations with traditional hospitals,
choosing instead to devote more time
to their own ambulatory treatment and
surgery centers or specialty hospitals in
which they have equity interests. These
facilities offer the potential for physicians
to generate higher incomes by sharing in
facility profits. The drawback is that the
growth of specialty facilities threatens
traditional hospitals with the loss of profitable
services and, as a result, limits their
ability to sustain cross-subsidies essential
for financing less profitable lines of business.
Moreover, to avoid seeing uninsured
patients for whom they will not be reimbursed,
some specialists have stopped
providing emergency room coverage
in Phoenix. Hospitals report that it is
increasingly difficult to provide on-call
coverage for certain specialties, and they
say that some specialists are banding
together in "cartel-like" arrangements
to demand above-market reimbursement
from hospitals for their services. Specialists’
decisions not to provide emergency room
coverage may have gained impetus from
regulations under the federal Emergency
Medical Treatment and Labor Act, which
imposes hefty fines if a physician or hospital
inappropriately transfers a medically
unstable patient to another facility for any
reason, including inability to pay.
Relationships between physicians
and health plans in Phoenix have also
become very contentious in the past two
years. On the heels of financial difficulties
that many attribute largely to managed
care, physicians increasingly are refusing
to enter into risk contracts with health
plans, and health plans are reverting to
fee-for-service payment. Meanwhile,
nearly every attempt at building organizations
to allow physicians to accept risk
has failed, leaving dim prospects for risk
contracting in the future. hysicians’ discontent with the local
health care system has reached new
heights over the past two years, and
physicians are aggressively pursuing
strategies to improve their financial
situations. Perhaps most significant,
some specialists have cut back on their
affiliations with traditional hospitals,
choosing instead to devote more time
to their own ambulatory treatment and
surgery centers or specialty hospitals in
which they have equity interests. These
facilities offer the potential for physicians
to generate higher incomes by sharing in
facility profits. The drawback is that the
growth of specialty facilities threatens
traditional hospitals with the loss of profitable
services and, as a result, limits their
ability to sustain cross-subsidies essential
for financing less profitable lines of business.
Moreover, to avoid seeing uninsured
patients for whom they will not be reimbursed,
some specialists have stopped
providing emergency room coverage
in Phoenix. Hospitals report that it is
increasingly difficult to provide on-call
coverage for certain specialties, and they
say that some specialists are banding
together in "cartel-like" arrangements
to demand above-market reimbursement
from hospitals for their services. Specialists’
decisions not to provide emergency room
coverage may have gained impetus from
regulations under the federal Emergency
Medical Treatment and Labor Act, which
imposes hefty fines if a physician or hospital
inappropriately transfers a medically
unstable patient to another facility for any
reason, including inability to pay.
Relationships between physicians
and health plans in Phoenix have also
become very contentious in the past two
years. On the heels of financial difficulties
that many attribute largely to managed
care, physicians increasingly are refusing
to enter into risk contracts with health
plans, and health plans are reverting to
fee-for-service payment. Meanwhile,
nearly every attempt at building organizations
to allow physicians to accept risk
has failed, leaving dim prospects for risk
contracting in the future.
Health Plans Seek to Regain Profitability
 ealth plans’ profitability has eroded
considerably in Phoenix since 1998,
a situation that has led to rising premiums
and instability in the health plan
market. Of the 10 commercial health
maintenance organizations (HMOs)
currently operating in Phoenix, only
two-Cigna and PacifiCare-are reportedly
profitable. Health plans in Phoenix
once relied on a strategy of increasing
their market share by keeping premiums
low. Like other health plans nationally,
however, many of them have concluded
that this strategy is unsustainable and
are increasing premiums and eliminating
unprofitable or marginal lines of business
to improve their financial condition.
Individuals with coverage from large
employers appear to have been largely
sheltered from health plans’ premium
increases. In the tight labor market
(currently under 3 percent unemployment),
most large firms have sought to
absorb the added costs or make only
minor changes to benefit structures,
viewing increased out-of-pocket costs
for their employees as a last resort.
Observers note, however, that small
employers-which account for the vast
majority of Phoenix area workplaces-
have been more likely to change health
plans to get a better price or to drop
coverage for employees altogether if they
are unable to find affordable rates. This
trend has significant implications in a
market where more than 25 percent of
the population already goes without
health insurance.
Health plans’ recent financial problems
have prompted the Arizona
Department of Insurance (DOI) to
place two plans, UnitedHealthcare and
Intergroup, on a "watch" status to monitor
their performance more closely. DOI’s
actions are attributed to criticism the
agency received for not adequately monitoring
the financial condition of Premier
Healthcare, a small provider-sponsored
HMO that became insolvent and went
into receivership in November 1999.
Problems with plans failing to pay
providers on time have also prompted
increased scrutiny by DOI, resulting in
fines for some plans.
DOI’s recent interventions reflect
an increasingly regulated health plan
environment that has emerged in Arizona
and nationally. In 1999, the Arizona legislature
enacted an HMO reform law giving
patients various rights to appeal their
health plan’s decisions, including the
right to sue their health plan. The list
of legislatively mandated health plan
benefits, which continues to grow, now
includes cancer clinical trials and chiropractic
services. Under a new state law
that takes effect this year, Arizona’s
bifurcated system of managed care
oversight will be eliminated, and the
health delivery and quality monitoring
responsibilities of the Department of
Health Services will be transferred to DOI.
Health plan respondents claim that Arizona’s new managed care regulations are
increasing costs, resulting in higher premiums for consumers. Other respondents
assert, however, that the regulations are needed to ensure that patient care and
provider payment are protected adequately in a managed care environment. ealth plans’ profitability has eroded
considerably in Phoenix since 1998,
a situation that has led to rising premiums
and instability in the health plan
market. Of the 10 commercial health
maintenance organizations (HMOs)
currently operating in Phoenix, only
two-Cigna and PacifiCare-are reportedly
profitable. Health plans in Phoenix
once relied on a strategy of increasing
their market share by keeping premiums
low. Like other health plans nationally,
however, many of them have concluded
that this strategy is unsustainable and
are increasing premiums and eliminating
unprofitable or marginal lines of business
to improve their financial condition.
Individuals with coverage from large
employers appear to have been largely
sheltered from health plans’ premium
increases. In the tight labor market
(currently under 3 percent unemployment),
most large firms have sought to
absorb the added costs or make only
minor changes to benefit structures,
viewing increased out-of-pocket costs
for their employees as a last resort.
Observers note, however, that small
employers-which account for the vast
majority of Phoenix area workplaces-
have been more likely to change health
plans to get a better price or to drop
coverage for employees altogether if they
are unable to find affordable rates. This
trend has significant implications in a
market where more than 25 percent of
the population already goes without
health insurance.
Health plans’ recent financial problems
have prompted the Arizona
Department of Insurance (DOI) to
place two plans, UnitedHealthcare and
Intergroup, on a "watch" status to monitor
their performance more closely. DOI’s
actions are attributed to criticism the
agency received for not adequately monitoring
the financial condition of Premier
Healthcare, a small provider-sponsored
HMO that became insolvent and went
into receivership in November 1999.
Problems with plans failing to pay
providers on time have also prompted
increased scrutiny by DOI, resulting in
fines for some plans.
DOI’s recent interventions reflect
an increasingly regulated health plan
environment that has emerged in Arizona
and nationally. In 1999, the Arizona legislature
enacted an HMO reform law giving
patients various rights to appeal their
health plan’s decisions, including the
right to sue their health plan. The list
of legislatively mandated health plan
benefits, which continues to grow, now
includes cancer clinical trials and chiropractic
services. Under a new state law
that takes effect this year, Arizona’s
bifurcated system of managed care
oversight will be eliminated, and the
health delivery and quality monitoring
responsibilities of the Department of
Health Services will be transferred to DOI.
Health plan respondents claim that Arizona’s new managed care regulations are
increasing costs, resulting in higher premiums for consumers. Other respondents
assert, however, that the regulations are needed to ensure that patient care and
provider payment are protected adequately in a managed care environment.
Seniors Face Fewer Choices and Higher Costs
 hoenix is one of the strongest Medicare
managed care markets in the country.
Zero dollar premiums and generous
benefit packages, including pharmaceutical
coverage, have attracted 168,000 local
Medicare beneficiaries (42 percent) to
Medicare+Choice HMOs. Recently, however,
the struggle by Phoenix health plans
to restore profitability has led some health
plans to withdraw from Medicare+Choice.
Other plans have instituted premiums
and/or reduced benefits in their Medicare
HMOs, leaving seniors with fewer choices
and higher out-of-pocket costs.
Since 1998, two health plans
have dropped out of the Phoenix
Medicare+Choice market. The withdrawal
of UnitedHealthcare and Blue
Cross Blue Shield of Arizona affected
20,000 Medicare beneficiaries, most of
whom are thought to have enrolled in
other HMOs. Though seven other
plans are expected to participate in the
Medicare+Choice market in 2001, these
plans say that low payment rates, coupled
with Balanced Budget Act imposed rate
ceilings that are significantly below medical
cost trends, limit their ability to make
long-term participation commitments.
Furthermore, health plans that
remain in the Phoenix Medicare+Choice
market are requiring seniors to contribute
more to the cost of care. Seniors who
previously paid no premiums in most
Medicare+Choice plans now face monthly
premiums of $25 or more, higher copayments
and more restrictive caps on
prescription drug coverage. Despite these
changes, demand for Medicare+Choice
plans in Phoenix remains strong, especially
among the area’s many young and
healthy retirees and individuals who want
the prescription drug benefit. Health
plans contend that they have no recourse
other than to increase beneficiary contributions
and reduce benefits if they are
to continue to participate in the
Medicare+Choice program and
remain financially sound.
Some health plans are considering
alternative Medicare products such as
preferred provider organizations (PPOs),
but so far no new managed care products
have been introduced into the market.
Recently, Sterling Life Insurance Company
began marketing a Medicare private fee-for-
service product in Phoenix. It is too
soon to determine what, if any, impact
such fee-for-service products will have
on the market. hoenix is one of the strongest Medicare
managed care markets in the country.
Zero dollar premiums and generous
benefit packages, including pharmaceutical
coverage, have attracted 168,000 local
Medicare beneficiaries (42 percent) to
Medicare+Choice HMOs. Recently, however,
the struggle by Phoenix health plans
to restore profitability has led some health
plans to withdraw from Medicare+Choice.
Other plans have instituted premiums
and/or reduced benefits in their Medicare
HMOs, leaving seniors with fewer choices
and higher out-of-pocket costs.
Since 1998, two health plans
have dropped out of the Phoenix
Medicare+Choice market. The withdrawal
of UnitedHealthcare and Blue
Cross Blue Shield of Arizona affected
20,000 Medicare beneficiaries, most of
whom are thought to have enrolled in
other HMOs. Though seven other
plans are expected to participate in the
Medicare+Choice market in 2001, these
plans say that low payment rates, coupled
with Balanced Budget Act imposed rate
ceilings that are significantly below medical
cost trends, limit their ability to make
long-term participation commitments.
Furthermore, health plans that
remain in the Phoenix Medicare+Choice
market are requiring seniors to contribute
more to the cost of care. Seniors who
previously paid no premiums in most
Medicare+Choice plans now face monthly
premiums of $25 or more, higher copayments
and more restrictive caps on
prescription drug coverage. Despite these
changes, demand for Medicare+Choice
plans in Phoenix remains strong, especially
among the area’s many young and
healthy retirees and individuals who want
the prescription drug benefit. Health
plans contend that they have no recourse
other than to increase beneficiary contributions
and reduce benefits if they are
to continue to participate in the
Medicare+Choice program and
remain financially sound.
Some health plans are considering
alternative Medicare products such as
preferred provider organizations (PPOs),
but so far no new managed care products
have been introduced into the market.
Recently, Sterling Life Insurance Company
began marketing a Medicare private fee-for-
service product in Phoenix. It is too
soon to determine what, if any, impact
such fee-for-service products will have
on the market.
Arizona Citizens Press for Aid for Large Uninsured Population
 he Phoenix area has one of the highest
rates of uninsurance in the country, with
more than one-quarter of the population
lacking coverage. Only 60 percent of
working adults and their dependents
receive health insurance through their
employers, and the preponderance of
low-wage jobs in the local employment
sector makes it likely that many people
cannot afford to purchase insurance on
their own. Federal welfare reform legislation
enacted in 1996 has contributed to
the insurance coverage problem, because
reportedly large numbers of former
welfare recipients who remain eligible
for Medicaid have not reenrolled. Arizona’s
State Child Health Insurance Program
(SCHIP), KidsCare, was implemented in
November 1998, and roughly 80,000 children
have gained coverage as a result of
KidsCare outreach efforts-half through
Medicaid and half through SCHIP. State
officials had originally hoped to enroll
60,000 children in KidsCare alone and
are now stepping up efforts to reach
this population.
Historically, Arizona’s political
climate has not been supportive of
state-sponsored initiatives to provide
funding for the uninsured, but in recent
years, Arizona citizens have used state
ballot initiatives to force the hand of the
legislature to address the insurance
coverage problem. An Arizona state ballot
initiative passed in 1994 created a tobacco
tax, with 70 percent of the revenues
dedicated to subsidizing health care for
the uninsured. Currently, these tobacco
tax revenues are the only source of funding
that can be used to provide care for
undocumented immigrants in Phoenix
and elsewhere in the state. With health
care costs continuing to escalate, however,
there are concerns that tobacco tax
revenues will not keep pace with the
health care needs of the large number
of uninsured persons.
In November 2000, Arizona citizens
passed two competing state ballot initiatives-
Proposition 200 and Proposition
204-that earmark the state’s $3.1 billion
tobacco settlement monies to expand
coverage to the population without health
insurance. Proposition 204 had the most
votes and was recently approved by federal
officials. The new funding will expand
Medicaid eligibility by raising the income
ceiling for eligibility to 100 percent of the
federal poverty level, extending coverage
to 130,000-180,000 Arizona residents
who lack health insurance-a 30 percent
increase over current Medicaid enrollment.
Despite the pressures of a large
uninsured population, the Phoenix
safety net has been relatively stable, but
that stability may now be in jeopardy.
Four downtown hospitals-the county-owned
Maricopa Integrated Health
System (MIHS), Good Samaritan, St.
Joseph’s and Phoenix Memorial-
provide care for the uninsured, as
does an extensive network of community
health clinics (CHCs) in Phoenix.
Market observers report that uninsured
individuals have reasonably good access
to primary care through the CHCs,
either by appointment or on a walk-in
basis. Securing specialty and inpatient
care through the CHCs, however, is
reportedly more difficult. To link
uninsured individuals with specialty
or inpatient care, CHCs rely largely
on relationships they have established
with providers in the community.
Some respondents express concern
that access to care for the uninsured
is deteriorating at MIHS. In 1994,
following substantial losses that threatened
its continued existence, MIHS
entered into a management agreement
with the for-profit hospital management
company, Quorum Health Resources.
Quorum has been successful in helping
to restore profitability to the county-owned
system, which reportedly now
has a surplus in excess of $18 million.
Although MIHS’s improved financial
condition may help to stabilize the
system as a key provider of care for
the uninsured, some respondents
speculate that its financial turnaround
has been the result of a decline in the
amount of uncompensated care the
system provides.
Consistent with these reports, other hospitals have noted significant increases
in emergency room use by uninsured persons. Some observers fear that this situation
will worsen under MIHS’s plan to shed its county hospital image by obtaining state
authorization to form a hospital district. This change will enable MIHS to compete
for a broader base of business, but some observers worry that it may also undermine
MIHS’s commitment to serve the uninsured. he Phoenix area has one of the highest
rates of uninsurance in the country, with
more than one-quarter of the population
lacking coverage. Only 60 percent of
working adults and their dependents
receive health insurance through their
employers, and the preponderance of
low-wage jobs in the local employment
sector makes it likely that many people
cannot afford to purchase insurance on
their own. Federal welfare reform legislation
enacted in 1996 has contributed to
the insurance coverage problem, because
reportedly large numbers of former
welfare recipients who remain eligible
for Medicaid have not reenrolled. Arizona’s
State Child Health Insurance Program
(SCHIP), KidsCare, was implemented in
November 1998, and roughly 80,000 children
have gained coverage as a result of
KidsCare outreach efforts-half through
Medicaid and half through SCHIP. State
officials had originally hoped to enroll
60,000 children in KidsCare alone and
are now stepping up efforts to reach
this population.
Historically, Arizona’s political
climate has not been supportive of
state-sponsored initiatives to provide
funding for the uninsured, but in recent
years, Arizona citizens have used state
ballot initiatives to force the hand of the
legislature to address the insurance
coverage problem. An Arizona state ballot
initiative passed in 1994 created a tobacco
tax, with 70 percent of the revenues
dedicated to subsidizing health care for
the uninsured. Currently, these tobacco
tax revenues are the only source of funding
that can be used to provide care for
undocumented immigrants in Phoenix
and elsewhere in the state. With health
care costs continuing to escalate, however,
there are concerns that tobacco tax
revenues will not keep pace with the
health care needs of the large number
of uninsured persons.
In November 2000, Arizona citizens
passed two competing state ballot initiatives-
Proposition 200 and Proposition
204-that earmark the state’s $3.1 billion
tobacco settlement monies to expand
coverage to the population without health
insurance. Proposition 204 had the most
votes and was recently approved by federal
officials. The new funding will expand
Medicaid eligibility by raising the income
ceiling for eligibility to 100 percent of the
federal poverty level, extending coverage
to 130,000-180,000 Arizona residents
who lack health insurance-a 30 percent
increase over current Medicaid enrollment.
Despite the pressures of a large
uninsured population, the Phoenix
safety net has been relatively stable, but
that stability may now be in jeopardy.
Four downtown hospitals-the county-owned
Maricopa Integrated Health
System (MIHS), Good Samaritan, St.
Joseph’s and Phoenix Memorial-
provide care for the uninsured, as
does an extensive network of community
health clinics (CHCs) in Phoenix.
Market observers report that uninsured
individuals have reasonably good access
to primary care through the CHCs,
either by appointment or on a walk-in
basis. Securing specialty and inpatient
care through the CHCs, however, is
reportedly more difficult. To link
uninsured individuals with specialty
or inpatient care, CHCs rely largely
on relationships they have established
with providers in the community.
Some respondents express concern
that access to care for the uninsured
is deteriorating at MIHS. In 1994,
following substantial losses that threatened
its continued existence, MIHS
entered into a management agreement
with the for-profit hospital management
company, Quorum Health Resources.
Quorum has been successful in helping
to restore profitability to the county-owned
system, which reportedly now
has a surplus in excess of $18 million.
Although MIHS’s improved financial
condition may help to stabilize the
system as a key provider of care for
the uninsured, some respondents
speculate that its financial turnaround
has been the result of a decline in the
amount of uncompensated care the
system provides.
Consistent with these reports, other hospitals have noted significant increases
in emergency room use by uninsured persons. Some observers fear that this situation
will worsen under MIHS’s plan to shed its county hospital image by obtaining state
authorization to form a hospital district. This change will enable MIHS to compete
for a broader base of business, but some observers worry that it may also undermine
MIHS’s commitment to serve the uninsured.
Issues to Track
 apid population growth continues to shape the Phoenix health
care market, attracting national firms and helping them to attain a dominant position
among both hospitals and health plans. Consolidation and new partnerships have
helped to strengthen hospitals’ bargaining power relative to health plans during
the past two years, but shifts by some physicians from providing services through
traditional hospitals in favor of their own specialty facilities are adding to
hospitals’ financial pressures and disrupting coverage arrangements. Meanwhile,
health plans have been struggling to regain financial stability. The result has
been higher premiums, reduced benefits and fewer plans participating in Medicare+Choice.
Large numbers of Phoenix residents remain uninsured, and respondents worry that
further changes in the county- owned hospital system threaten to weaken the safety
net in the future.
As the Phoenix health care market continues to evolve, the following issues are
important to track: apid population growth continues to shape the Phoenix health
care market, attracting national firms and helping them to attain a dominant position
among both hospitals and health plans. Consolidation and new partnerships have
helped to strengthen hospitals’ bargaining power relative to health plans during
the past two years, but shifts by some physicians from providing services through
traditional hospitals in favor of their own specialty facilities are adding to
hospitals’ financial pressures and disrupting coverage arrangements. Meanwhile,
health plans have been struggling to regain financial stability. The result has
been higher premiums, reduced benefits and fewer plans participating in Medicare+Choice.
Large numbers of Phoenix residents remain uninsured, and respondents worry that
further changes in the county- owned hospital system threaten to weaken the safety
net in the future.
As the Phoenix health care market continues to evolve, the following issues are
important to track:
- What effects will contrary pressures- hospitals’ increasing negotiating
leverage with health plans and physicians shifting to specialty facilities-have
on hospital prices and overall health care costs?
- As health plans attempt to restore profitability by increasing premiums,
how will the low-wage market respond? Will employers shift the increased costs
to their employees? Will they drop coverage? Or will purchasers push for more
tightly managed products?
- What impact will changes by health plans in their Medicare products have
on the Phoenix market? Will Phoenix seniors see improved choice of plans,
lower costs and/or expanded benefits? Will seniors return to traditional fee-for-
service coverage?
- How will increased funding allocated under recent ballot initiatives affect
insurance coverage? Will the local safety net continue to have sufficient
capacity to serve the remaining uninsured?
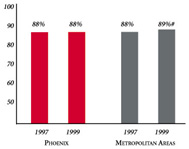
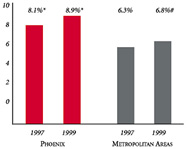
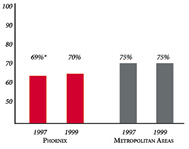
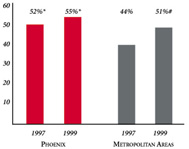
Phoenix’s Experience with the Local Health System, 1997 and 1999
Background and Observations
| Phoenix Demographics |
| Phoenix |
Metropolitan areas above 200,000 population |
Population, July 1, 19991
3,013,696 |
| Population Change, 1990-19992
|
| 35% |
8.6% |
| Median Income3 |
| $29,135 |
$27,843 |
| Persons Living in Poverty3 |
| 14% |
14% |
| Persons Age 65 or Older3 |
| 13% |
11% |
Sources:
1. US Bureau of Census, 1999 Community Population Estimates
2. US Bureau of Census, 1990 & 1999 Community Population Estimates
3. Community Tracking Study Household Survey, 1998-1999 |
| Health Insurance Status |
| Phoenix |
Metropolitan areas above 200,000 population |
| Persons under Age 65 with No Health Insurance1 |
| 17% |
15% |
| Children under Age 18 with No Health Insurance1
|
| 16% |
11% |
| Employees Working for Private Firms that
Offer Coverage2 |
| 86% |
84% |
| Average Monthly Premium for Self-Only Coverage
under Employer-Sponsored Insurance2 |
| $151 |
$181 |
Sources:
1. Community Tracking Study Household Survey, 1998-1999
2. Robert Wood Johnson Foundation Employer Health Insurance Survey, 1997 |
| Health System Characteristics |
| Phoenix |
Metropolitan areas above 200,000 population |
| Staffed Hospital Beds per 1,000 Population1
|
| 2.2 |
2.8 |
| Physicians per 1,000 Population2
|
| 1.7 |
2.3 |
| HMO Penetration, 19973 |
| 34% |
32% |
| HMO Penetration, 19994 |
| 34% |
36% |
Sources:
1. American Hospital Association, 1998
2. Area Resource File, 1998 (includes nonfederal, patient care physicians,
except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge 8.1
4. InterStudy Competitive Edge 10.1 |

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. Every two years, HSC conducts surveys in all 60
communities and site visits in 12 communities. The Community Report series documents
the findings from the third round of site visits. Analyses based on site visit
and survey data from the Community Tracking Study are published by HSC in Issue
Briefs, Data Bulletins and peer-reviewed journals. These publications are
available at www.hschange.org.
Authors of the Phoenix Community Report:
Debra A. Draper, Mathematica Policy Research, Inc.
Linda R. Brewster, HSC
Lawrence D. Brown, Columbia University
Carolyn A. Watts, University of Washington
Laurie E. Felland, HSC
Jon B. Christianson, University of Minnesota
Jeffrey Stoddard, HSC
Michael Park, HSC
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Ann C. Greiner
Editor: The Stein Group
|