
Even When Physicians Adopt E-Prescribing, Use of Advanced Features Lags
Issue Brief No. 133
July 2010
Joy M. Grossman
Physician practice adoption of electronic prescribing has not guaranteed that individual physicians will routinely use the technology, particularly the more advanced features the federal government is promoting with financial incentives, according to a new national study from the Center for Studying Health System Change (HSC). Slightly more than two in five physicians providing office-based ambulatory care reported that information technology (IT) was available in their practice to write prescriptions in 2008, the year before implementation of federal incentives. Among physicians with e-prescribing capabilities, about a quarter used the technology only occasionally or not at all. Moreover, fewer than 60 percent of physicians with e-prescribing had access to three advanced features included as part of the Medicare and Medicaid incentive programs—identifying potential drug interactions, obtaining formulary information and transmitting prescriptions to pharmacies electronically—and less than a quarter routinely used all three features. Physicians in practices using electronic medical records exclusively were much more likely to report routine use of e-prescribing than physicians with stand-alone e-prescribing systems. Other gaps in adoption and routine use of e-prescribing also exist, most notably between physicians in larger and smaller practices.
- Physician Electronic Prescribing Adoption and Use Limited
- ’Meaningful Use’ of Advanced Feartures Lags
- Electronic Medical Records and E-Prescribing
- E-Prescribing and Practice Size
- Achieving ’Meaningful Use’ of E-Precribing
- Notes
- Data Source and Funding Acknowledgement
Physician Electronic Prescribing Adoption and Use Limited
![]() ublic- and private-sector efforts to promote health IT have focused on e-prescribing—defined in this study as the use of IT to write prescriptions—because of the potential to improve patient safety and slow health care spending growth.1 To spur adoption, the federal government provides financial incentives to physicians who e-prescribe in ambulatory settings (see box below for more details). Medicare started paying bonuses in 2009 to qualifying e-prescribing physicians under the Medicare Improvements for Patients and Providers Act (MIPPA). And starting in 2011, under the American Recovery and Reinvestment Act (ARRA), eligible physicians who demonstrate “meaningful use” of electronic medical records (EMRs) for ambulatory care, including e-prescribing, can receive substantially larger incentives under either Medicare or Medicaid but not both. Eventually, eligible physicians who do not meet requirements under the Medicare incentive programs will face financial penalties.
ublic- and private-sector efforts to promote health IT have focused on e-prescribing—defined in this study as the use of IT to write prescriptions—because of the potential to improve patient safety and slow health care spending growth.1 To spur adoption, the federal government provides financial incentives to physicians who e-prescribe in ambulatory settings (see box below for more details). Medicare started paying bonuses in 2009 to qualifying e-prescribing physicians under the Medicare Improvements for Patients and Providers Act (MIPPA). And starting in 2011, under the American Recovery and Reinvestment Act (ARRA), eligible physicians who demonstrate “meaningful use” of electronic medical records (EMRs) for ambulatory care, including e-prescribing, can receive substantially larger incentives under either Medicare or Medicaid but not both. Eventually, eligible physicians who do not meet requirements under the Medicare incentive programs will face financial penalties.
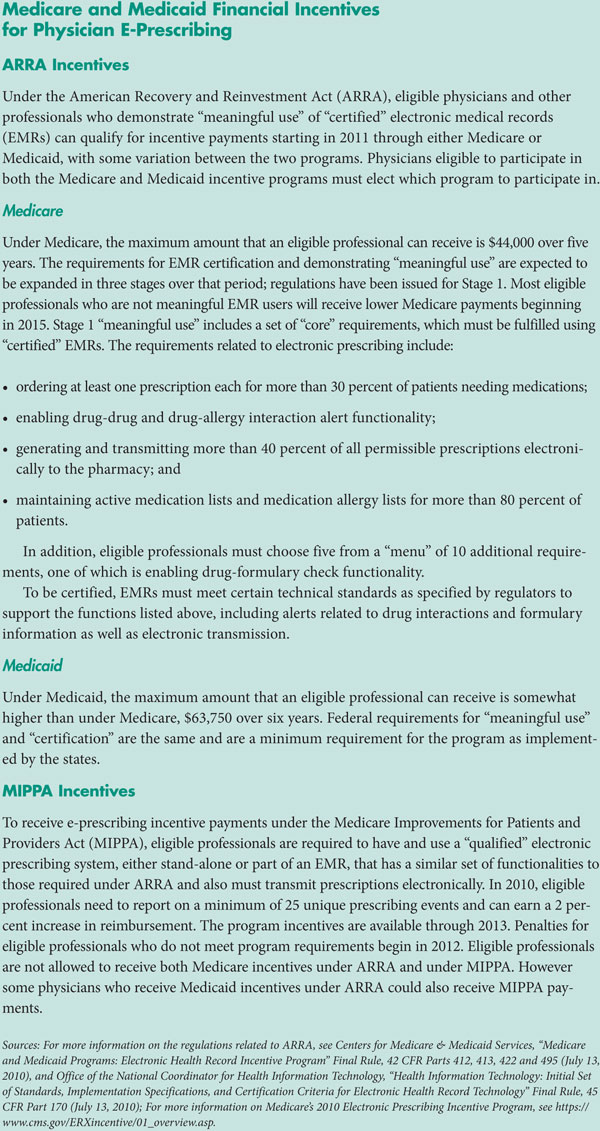
Baseline data from 2008, before implementation of federal incentive programs, show that, despite many earlier public- and private-sector initiatives, physician adoption and use of e-prescribing remained limited.2 Two in five physicians in office-based ambulatory practice (41.9%) reported that information technology was available in their practice to write prescriptions in 2008, according to HSC’s nationally representative Health Tracking Physician Survey (see Table 1 and Data Source). Moreover, physicians who had access to e-prescribing did not necessarily use it routinely. About a quarter of the physicians reporting availability of IT to write prescriptions (23.1%) used the technology only occasionally or not at all. So in 2008, about one-third of all physicians in ambulatory settings (32.3%) routinely used e-prescribing.
Back to Top
’Meaningful Use’ of Advanced Features Lags
![]() he core feature of e-prescribing systems—the capability to write and store prescriptions electronically—can provide physicians and patients with clearly documented medication lists that can help reduce prescribing errors and support care coordination. E-prescribing systems also provide pharmacies with computer-generated prescriptions that can help reduce errors in filling prescriptions resulting from poor handwriting or incomplete information.
he core feature of e-prescribing systems—the capability to write and store prescriptions electronically—can provide physicians and patients with clearly documented medication lists that can help reduce prescribing errors and support care coordination. E-prescribing systems also provide pharmacies with computer-generated prescriptions that can help reduce errors in filling prescriptions resulting from poor handwriting or incomplete information.
To capture the full benefits of e-prescribing, proponents believe physicians must routinely use advanced features, such as drug interaction alerts or patient formulary information. Such features provide physicians with additional information that may lead to different prescribing decisions. Direct electronic transmission of prescriptions from physician practice IT systems to pharmacy IT systems also reduces manual entry of prescriptions at pharmacies. Despite limited evidence on the effects of e-prescribing in ambulatory settings, some experts believe physicians’ use of these advanced features can reduce medical errors, improve physician practice and pharmacy efficiency, and increase formulary compliance and generic prescribing.3
Studies suggest, however, that substantial barriers to physician use of advanced e-prescribing features exist. E-prescribing systems may not have these advanced features, and, even if they do, practices may not implement them or physicians may not use them routinely for a variety of reasons.4 To help overcome these barriers, the federal government has included e-prescribing as part of the broader requirements to qualify for Medicare or Medicaid incentive payments under ARRA. Among other requirements, to qualify, physicians must have EMRs that are “certified” as having specific e-prescribing capabilities and demonstrate “meaningful use” of these certified systems for e-prescribing. Incentives for e-prescribing under MIPAA have similar requirements for IT system functionality and use, although the specifics differ from the ARRA requirements.
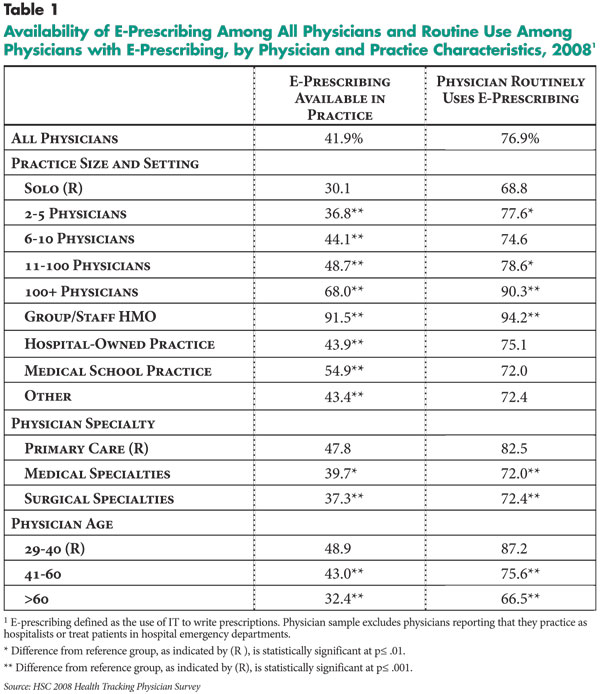
The HSC Health Tracking Physician Survey is the first nationally representative survey to report on physician access to and use of several of the advanced e-prescribing features included under MIPAA and ARRA incentive programs. These include features to: obtain information about potential drug interactions with other previously prescribed medications, a patient’s allergies, and/or patient conditions; obtain patient formulary information; and transmit prescriptions to pharmacies. According to the survey, these advanced features were not always available to physicians with e-prescribing capabilities, and, even when they were, physicians did not always use them routinely (see Figure 1).5
About two-thirds of physicians with IT to write prescriptions (64.5%) routinely used the drug interaction feature, slightly more than half (53.7%) routinely transmitted prescriptions to pharmacies and only 34.3 percent routinely used the formulary information feature. Only three in five physicians with IT to write prescriptions (59.4%) reported that all three features were available in their practice, and fewer than a quarter (22.7%) used all three routinely. So in 2008, only 9.6 percent of all physicians in office-based ambulatory settings routinely used the three advanced e-prescribing features.
Back to Top
Electronic Medical Records and E-Prescribing
![]() rescriptions can be written electronically using stand-alone e-prescribing systems or modules integrated into electronic medical records (EMRs). Stand-alone systems are less expensive and easier to implement than EMRs and are viewed as a potential gateway to full EMR adoption. In contrast, EMRs offer integration of e-prescribing into physician practice workflow and prescriber access to the full content of patient records, such as laboratory test results, when making prescribing decisions.
rescriptions can be written electronically using stand-alone e-prescribing systems or modules integrated into electronic medical records (EMRs). Stand-alone systems are less expensive and easier to implement than EMRs and are viewed as a potential gateway to full EMR adoption. In contrast, EMRs offer integration of e-prescribing into physician practice workflow and prescriber access to the full content of patient records, such as laboratory test results, when making prescribing decisions.
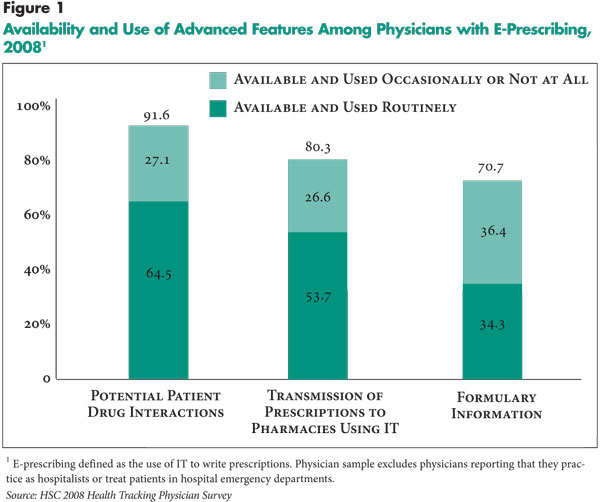
Of all physicians reporting access to IT to write prescriptions, about half (50.6%) reported that their practice used an EMR exclusively to manage patient records, 19.3 percent reported no EMR and the remaining 30.1 percent reported their practice used some mix of EMRs and paper records. For purposes of this analysis, physicians with IT to write prescriptions in practices using EMRs exclusively were assumed to use the e-prescribing module of the EMR and physicians in practices without an EMR were assumed to use stand-alone e-prescribing systems. Physicians in practices using a mix of EMR and paper records may use an EMR or a stand-alone system for e-prescribing.
Among physicians with IT to write prescriptions, those in practices that used EMRs exclusively were more than 1.5 times more likely to use electronic prescribing routinely than those with stand-alone systems (91.0% vs. 56.9%) (see Figure 2). Similarly, physicians in practices using EMRs were significantly more likely to use the advanced features routinely than physicians using stand-alone systems despite only small differences in availability of these e-prescribing features between the two groups (findings not shown). In fact, physicians in practices using EMRs were almost twice as likely as physicians using stand-alone systems to report using all three features routinely (29.6% vs. 15.5%).
E-Prescribing and Practice Size
![]() s with other health IT, physicians in larger practices were much more likely to report having IT to write prescriptions than other physicians. Physicians in group/staff health maintenance organizations (HMOs) reported the highest rate of adoption at 91.5 percent, a three-fold difference with physicians in solo practices who reported the lowest rate at 30.1 percent. Gaps in routine use were not always significant and were smaller when they were significant. Among physicians with e-prescribing, almost all physicians in HMOs (94.2%) reported using e-prescribing routinely in contrast to 68.8 percent of physicians in solo practices.
s with other health IT, physicians in larger practices were much more likely to report having IT to write prescriptions than other physicians. Physicians in group/staff health maintenance organizations (HMOs) reported the highest rate of adoption at 91.5 percent, a three-fold difference with physicians in solo practices who reported the lowest rate at 30.1 percent. Gaps in routine use were not always significant and were smaller when they were significant. Among physicians with e-prescribing, almost all physicians in HMOs (94.2%) reported using e-prescribing routinely in contrast to 68.8 percent of physicians in solo practices.
Gaps in access to and use of IT to write prescriptions also existed by physician specialty and age, although the gaps were smaller than for practice size. Medical and surgical specialists were somewhat less likely to adopt and routinely use e-prescribing than primary care physicians. Access to and use of IT to write prescriptions declined with age. Among physicians with IT to write prescriptions, two-thirds of physicians older than 60 (66.5%) routinely e-prescribed in contrast to 87.2 percent of the youngest physicians, aged 29 to 40.
At least some of the variation in adoption and use of electronic prescribing by practice size may be related to the higher rates of EMR adoption in larger practices. When considering only physicians in practices using EMRs exclusively, differences in rates of adoption and routine use of e-prescribing by practice size narrowed substantially (findings not shown). Similarly, older physicians may be less likely to have access to e-prescribing because they are more likely to work in smaller practices, which typically have less IT available.
Back to Top
Achieving ’Meaningful Use’ of E-Prescribing
![]() doption of e-prescribing remains low, particularly among the half of all physicians who work in solo or two- to five-physician practices. And, among physicians with e-prescribing capabilities, many do not use the technology routinely, and even fewer use advanced e-prescribing features routinely.
doption of e-prescribing remains low, particularly among the half of all physicians who work in solo or two- to five-physician practices. And, among physicians with e-prescribing capabilities, many do not use the technology routinely, and even fewer use advanced e-prescribing features routinely.
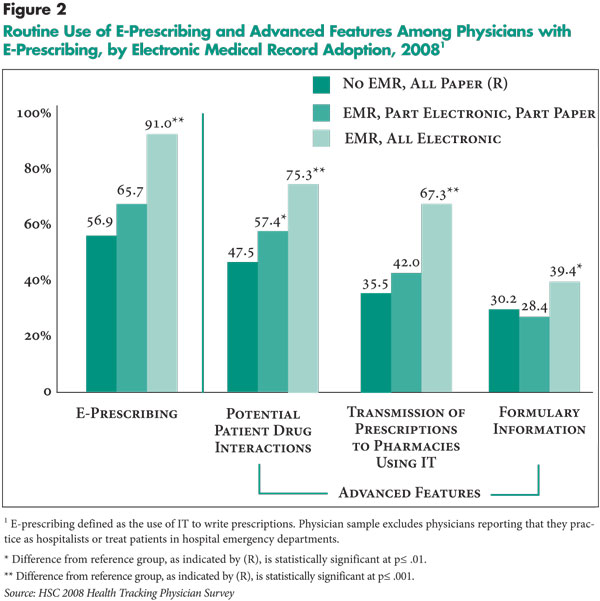
Federal incentive programs are being designed explicitly to help overcome barriers to effective use of e-prescribing and EMRs. Incentive payments are contingent on both having EMRs with advanced features meeting technical standards and achieving specified measures of use, as well as reporting on clinical quality. These requirements will be expanded in stages. For example, initially the use of two e-prescribing features will be measured—electronic prescription orders and electronic transmission of prescriptions to pharmacies.
In an encouraging sign, since the implementation of the MIPPA incentive program, Surescripts, which provides the main e-prescribing transmission network, reported that although the proportion of prescriptions transmitted electronically is still low, the number of prescriptions rose 181 percent and the percentage of prescribers transmitting prescriptions electronically more than doubled between 2008 and 2009.
Physician experiences with adoption and use of e-prescribing are a potential harbinger of the benefits and challenges federal policy makers will face in attempting to increase meaningful use of health IT. E-prescribing is one of the most mature forms of health IT and health information exchange, yet barriers to effective use remain. For example, the relatively low use of formulary information may reflect some physicians’ reluctance to rely on incomplete and what they perceive as inaccurate information.6 Similarly, many studies have shown that physicians experience “alert” fatigue given the current design of health IT systems, and such usability issues will need to be addressed to help maximize e-prescribing benefits.7 In addition, some retail and mail-order pharmacies currently do not use e-prescribing for some or all of their transactions.8 As these examples illustrate, a broader set of stakeholders beyond providers must be engaged to achieve effective use of health IT. Although the federal incentive programs and additional ARRA funding to help support health IT infrastructure development do not directly address these issues, to the extent that e-prescribing and use of EMRs become more widespread, other involved parties may have greater incentives to help resolve barriers.
Moreover, the challenges to implementation of EMRs as a whole are substantially more complex than e-prescribing. And, EMR technology is much less mature, suggesting that policy makers should expect a substantially longer time horizon to achieve meaningful use of health IT than the five- to six-year horizon of the Medicare and Medicaid incentive programs.
Back to Top
Notes
| 1. | Johnston, Doug, Eric Pan and Jan Walker, “The Value of Computerized Provider Order Entry in Ambulatory Settings,” The Journal of Healthcare Information Management, Vol. 18, No. 21 (Winter 2004). |
| 2. | Surescripts, Advancing Healthcare In America: 2009 National Progress Report On E-Prescribing (2010), available at http://www.surescripts.com/media/515306/2009_national-progress-report.pdf. |
| 3. | eHealth Initiative, Electronic Prescribing: Becoming Mainstream Practice (June 2008), available at http://www.ehealthinitiative.org/sites/default/files/eHI_CIMM_ePrescribing_Report_6-10-08_FINAL(1).pdf. |
| 4. | Grossman, Joy M., et al., “Physicians’ Experiences Using Commercial E-prescribing Systems,” Health Affairs, Web exclusive (April 3, 2007); National Opinion Research Center (NORC) at the University of Chicago, Findings from the Evaluation of E-Prescribing Pilot Sites, AHRQ Publication No. 07-0047-EF, Rockville, Md. (April 2007); Wang, C. Jason, et al., “Perceptions of Standards-Based Electronic Prescribing Systems as Implemented in Outpatient Primary Care: A Physician Survey,” Journal of the American Medical Informatics Association, Vol.16, No. 4 (July-August 2009). |
| 5. | Survey estimates of availability and use of advanced features to transmit prescriptions to pharmacies likely overstate the proportion of physicians in 2008 that would have met federal requirements for electronic transmission of prescriptions between prescriber and pharmacy IT systems. Given the wording of the survey question, estimates may include physicians who send prescriptions via computerized fax only, which would not meet federal requirements. The survey found 28.4 percent of all office-based physicians transmitted prescriptions using IT in 2008 (findings not shown). In contrast, Surescripts, the vendor that provides the main e-prescribing transmission network, which meets federal requirements, reported that at the end of 2008, only 12.1 percent of office-based physicians transmitted prescriptions using its network, rising to 26 percent at the end of 2009. See Surescripts, 2008 National Progress Report on E-prescribing (2009) and Surescripts (2010). |
| 6. | Surescripts (2010); Wang (2009). |
| 7. | eHealth Initiative (2008). |
| 8. | Surescripts (2010). |
Back to Top
Data Source
This Issue Brief presents findings from the HSC 2008 Health Tracking Physician Survey, a nationally representative mail survey of U.S. physicians providing at least 20 hours per week of direct patient care. The sample of physicians was drawn from the American Medical Association master file and included active, nonfederal, office- and hospital-based physicians. Residents and fellows were excluded, as well as radiologists, anesthesiologists and pathologists. The survey includes responses from more than 4,700 physicians, and the response rate was 62 percent. Because this Issue Brief focuses on electronic prescribing in physician offices, physicians reporting that they practice as hospitalists or treat patients in hospital emergency departments were excluded from this study. The resulting study sample is 4,182 physicians. More detailed information on survey content and methodology can be found at www.hschange.org.
Physicians were asked “Is information technology available in your practice to: (1) write prescriptions, (2) transmit prescriptions to the pharmacy, (3) obtain information on potential patient drug interactions with other drugs, allergies, and/or patient conditions, and (4) obtain information on formularies,” among other clinical activities. If the response was “yes,” physicians were asked “How often do you personally use the technology?” The response categories provided were “routinely,” “occasionally” or “not at all.” Physicians were also asked, “Does your main practice use electronic medical records?” The response categories were “yes, all electronic,” “yes, part electronic and part paper,” and “no, all paper.”
Funding Acknowledgement:
The 2008 HSC Health Tracking Physician Survey and this research were funded by the Robert Wood Johnson Foundation.
Back to Top
RESEARCH BRIEFS are published by the Center for Studying Health System
Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org