
Modest and Uneven: Physician Efforts to Reduce Racial and Ethnic Disparities
Issue Brief No. 130
February 2010
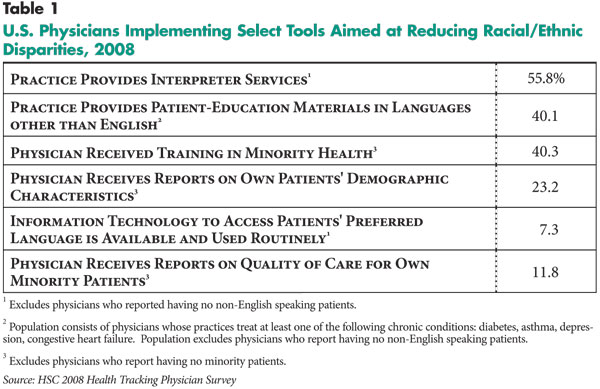
James D. Reschovsky, Ellyn R. Boukus
While nearly half of U. S. physicians identify language or cultural communication barriers as obstacles to providing high-quality care, physician adoption of practices to overcome such barriers is modest and uneven, according to a new national study by the Center for Studying Health System Change (HSC). Despite broad consensus among the medical community about how physicians can help to address and, ultimately, reduce racial and ethnic disparities, physician adoption of several recommended practices to improve care for minority patients ranges from 7 percent reporting they have the capability to track patients’ preferred language to 40 percent reporting they have received training in minority health issues to slightly more than half reporting their practices provide some interpreter services. The challenges physicians face in providing quality health care to all of their patients will keep mounting as the U.S. population continues to diversify and the minority population increases.
- Physicians’ Role in Addressing Racial and Ethnic Disparities
- Reducing Language and Cultural Barriers
- Information Feedback to Physicians
- Addressing Disparities Varies by Practice Characteristics
- Policy Implications
- Notes
- Data Source and Funding Acknowledgement
Physicians’ Role in Addressing Racial and Ethnic Disparities
![]() eginning in 2003, the federal government through the National Healthcare Disparities Report has annually documented wide disparities in the quality of health care received by different racial and ethnic groups in the United States. And, little progress has been made in closing these quality gaps, according to the latest report issued in May 2009.
eginning in 2003, the federal government through the National Healthcare Disparities Report has annually documented wide disparities in the quality of health care received by different racial and ethnic groups in the United States. And, little progress has been made in closing these quality gaps, according to the latest report issued in May 2009.
Although differences in insurance coverage and other patient, community and health system factors contribute to disparities, studies indicate disparities also can arise during the patient-physician encounter.1 The Institute of Medicine and the National Quality Forum, among others, have outlined measures physicians and physician practices can take: 1) to reduce language and cultural barriers that hinder communication between some minority patients and their physicians; and 2) to establish practice-level information systems to facilitate the elimination of language and cultural barriers and provide feedback on the quality of care provided across racial and ethnic groups.2
Drawing on these recommendations, the nationally representative 2008 HSC Health Tracking Physician Survey asked physicians about steps they and their practices have taken to reduce language and cultural barriers and generate information at the practice level to improve care for minority patients (see Data Source). The survey asked physicians the following:
- whether their practice provides interpreter services;
- whether their practice provides patient-education materials in languages other than English;
- whether they have received training in minority health issues;
- whether they receive reports containing patient demographic information, such as race or ethnicity;
- whether their practice has information technology (IT) to identify patients’ preferred language; and
- whether they receive reports about the quality of care delivered to minority patients.
Back to Top
Reducing Language and Cultural Barriers
![]() prerequisite for quality medical care is effective communication between patient and caregiver. Nearly half (48.6%) of all U.S. physicians in 2008 reported that difficulty communicating with patients because of language or cultural barriers was at least a minor problem affecting their ability to provide quality care, though less than 5 percent viewed it as a major problem. The failure of physicians to address communication barriers, coupled with the potential ineffectiveness of measures taken, may contribute to disparities in the quality of care across racial and ethnic groups.
prerequisite for quality medical care is effective communication between patient and caregiver. Nearly half (48.6%) of all U.S. physicians in 2008 reported that difficulty communicating with patients because of language or cultural barriers was at least a minor problem affecting their ability to provide quality care, though less than 5 percent viewed it as a major problem. The failure of physicians to address communication barriers, coupled with the potential ineffectiveness of measures taken, may contribute to disparities in the quality of care across racial and ethnic groups.
Interpreter services. An ever-increasing number of people in the United States speak a language other than English at home (56 million people aged 5 and older in 2008, 44% of whom reported they speak English less than “very well”).3 These facts highlight the need for interpreter services to improve the quality of care for patients with limited-English proficiency.4
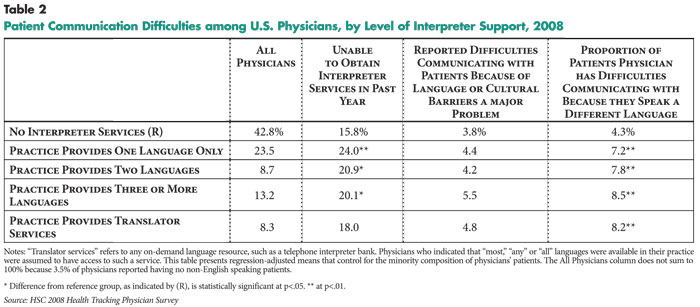
Moreover, providers have legal obligations to provide needed interpreter services, at least for patients with public insurance. While nearly 97 percent of physicians have at least some non-English speaking patients, only slightly more than half of physicians (56%) were in practices that provided interpreter services in 2008 (see Table 1). Of physicians in practices that provided interpreter services, 44 percent were in practices that offered interpretation in only one language, 16 percent were in practices offering two languages, with the rest in practices providing interpretation in three or more languages, including telephonic translation services.
Interestingly, among physicians with patients who speak different languages, those in practices providing interpreter services were more likely to report communication difficulties than those without access to interpreter services, even after adjusting for the percentage of minority patients treated (see Table 2). While this may reflect greater demand for interpreter services among practices experiencing language barrier problems, it also may indicate that interpreter services are not always readily available or are inadequate.5 Nearly one in five physicians (18.8%) reported being unable to obtain interpreter services in the past 12 months that they believed were medically necessary. Moreover, of physicians reporting that their practices provided interpreter services, it is unclear how many provide professional interpretation services, as opposed to using staff members who may be less than fluent in the language, unfamiliar with medical terminology or unaware of cultural nuances.
Non-English, written patient-education materials. Low health literacy—defined as limited capacity to obtain, process and understand health information and services needed to make appropriate decisions6—is associated with less use of preventive services, more frequent hospital and emergency department visits, and poorer health.7 Minorities, particularly those not proficient in English, are disproportionately represented among individuals with low health literacy.
Although other care management practices have been found to be more effective than written materials in educating and engaging patients in their own self-care, physicians can help promote health literacy by providing patients with written information about their conditions and self-care instructions.8 Offering patient-education materials in appropriate languages for patients with limited-English proficiency also can promote health literacy. Among physicians in practices treating patients with any of four prevalent chronic conditions—asthma, diabetes, congestive heart failure and depression—72 percent in 2008 reported their practice provides patient-education materials for at least one of the four conditions.9 Yet, only 40 percent of physicians in these practices reported providing patient-education materials in languages other than English for at least one of the conditions.
Physician training in minority health. Culturally competent care emphasizes comprehension of cultural differences and the interaction with individuals’ health expectations and behaviors, disease incidence and prevalence, and treatment outcomes. The goal of minority health education is to develop practitioner skills to tailor care to patients’ culturally unique needs.10 Roughly four in 10 physicians in 2008 reported they have received some training in minority health, such as cultural competency training, through professional meetings, workshops or continuing medical education courses. However, the survey question did not assess the nature of the training, its comprehensiveness or how recently it was received. Although more likely to have received training in minority health than other physicians, only half of physicians in high-minority practices (defined as 50% or more minority patients) had received such training.
Back to Top
 >
>Information Feedback to Physicians
![]() ther prerequisites for improving care for minority patients include identifying them, knowing what language they prefer and monitoring what quality of care they receive. Although such information could exist in purely paper recordkeeping systems, recent national efforts have focused on electronic medical records (EMRs). Movement in this direction is likely to accelerate in the near future because of incentives in the American Recovery and Reinvestment Act of 2009 and emerging guidelines from the Office of the National Coordinator for Health Information Technology and the Centers for Medicare and Medicaid Services that include these capabilities in definitions of “meaningful use” of EMRs qualifying for subsidies.
ther prerequisites for improving care for minority patients include identifying them, knowing what language they prefer and monitoring what quality of care they receive. Although such information could exist in purely paper recordkeeping systems, recent national efforts have focused on electronic medical records (EMRs). Movement in this direction is likely to accelerate in the near future because of incentives in the American Recovery and Reinvestment Act of 2009 and emerging guidelines from the Office of the National Coordinator for Health Information Technology and the Centers for Medicare and Medicaid Services that include these capabilities in definitions of “meaningful use” of EMRs qualifying for subsidies.
Reporting of patient demographic information and access to patient-preferred language. Less than one in four physicians (23%) indicated they receive reports on patient demographics. Among physicians in high-minority practices, only a slightly higher percentage (29%) received demographic reports.
Knowing what language a patient prefers is important for arranging and coordinating interpreter services for patients with limited-English proficiency or matching appropriate physicians to patients. Twenty-two percent of physicians indicated their practice has IT capable of reporting patients’ preferred language (findings not shown), but only a third of these physicians (7%) routinely used this capability.
Reporting of quality of care delivered to minority patients. Nearly nine out of 10 physicians lacked a formal means to assess the quality of care provided to patients across racial and ethnic groups. Only 11.8 percent of physicians reported access to reports on the quality of care they provide stratified by patient race or ethnicity.
Addressing Disparities Varies by Practice Characteristics
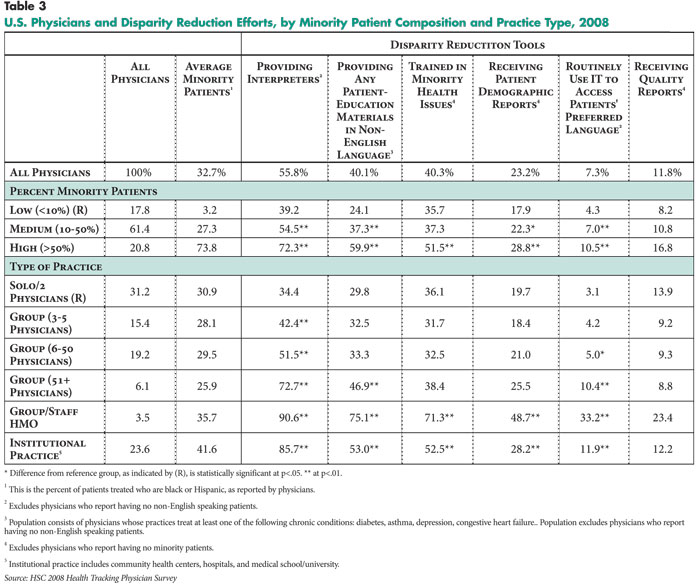
![]() doption rates vary not only across the different tools,
but also according to practice characteristics (see Table
3).11 Physicians in practices with a greater share
of minority patients were more likely to adopt each of the measures to address
disparities. For example, almost twice as many physicians reported providing
interpreter services in practices with a majority of minority patients, relative
to those in low-minority practices—less than 10 percent minority patients (72.3%
vs. 39.2%). Similarly, there were large differences in provision of patient-education
materials in foreign languages (60% vs. 24%), routine use of IT to access patients’
preferred languages (10.5% vs. 4.3%) and quality reporting by racial or ethnic
group (16.8% vs. 8.2%).
doption rates vary not only across the different tools,
but also according to practice characteristics (see Table
3).11 Physicians in practices with a greater share
of minority patients were more likely to adopt each of the measures to address
disparities. For example, almost twice as many physicians reported providing
interpreter services in practices with a majority of minority patients, relative
to those in low-minority practices—less than 10 percent minority patients (72.3%
vs. 39.2%). Similarly, there were large differences in provision of patient-education
materials in foreign languages (60% vs. 24%), routine use of IT to access patients’
preferred languages (10.5% vs. 4.3%) and quality reporting by racial or ethnic
group (16.8% vs. 8.2%).
Weighting physicians by the proportion of minority patients they treat allows a rough estimate of the distribution of minority patients treated by physicians using various tools to reduce disparities. For example, while 56 percent of physicians provided interpreter services, 64 percent of minority patients were treated by physicians in practices with interpreter services. And, 14 percent of minority patients were treated by physicians who received reports on the quality of care for minority patients (findings not shown).
Apart from the minority composition of physicians’ patient panels, practice type also demonstrates a strong association with efforts to address disparities.12 Physicians in solo and group practices were less likely to adopt measures to address disparities than those in institutional practices, such as hospitals, health maintenance organizations (HMOs) and medical schools. For example, nearly 90 percent of physicians in group- or staff-model HMOs reported providing interpreter services, compared with 34 percent of physicians in solo or two-physician practices. Physicians in HMOs also were more than 10 times as likely as those in solo or two-physician practices to routinely use IT to access information on patients’ preferred language.
Back to Top
Policy Implications
![]() espite broad consensus among the medical community about how physicians can help to address and, ultimately, reduce disparities, physician adoption of several recommended practices to improve care for minority patients remains low. Cost and lack of reimbursement for these activities are likely among the largest obstacles to implementation in physician practices.
espite broad consensus among the medical community about how physicians can help to address and, ultimately, reduce disparities, physician adoption of several recommended practices to improve care for minority patients remains low. Cost and lack of reimbursement for these activities are likely among the largest obstacles to implementation in physician practices.
The tools most commonly adopted tend to be the least expensive to implement: provision of patient-education materials in foreign languages, which can often be downloaded from the Internet for free, and training in minority health. On the other hand, IT systems that can support reporting on patient care by race, ethnicity or language, as well as interpreter services, are expensive and less common. For instance, an encounter with an interpreter involves the cost of paying the interpreter and requires the physician to spend more time with the patient—time that could have been devoted to seeing more patients. Larger physician organizations and those with higher concentrations of patients needing interpretation services can take advantage of scale economies to more efficiently provide these services. This may help to explain their higher adoption rates relative to solo and small-group practices.
Competent interpreter services are a key step in improving physician-patient communication when language barriers are a problem. Under federal law—Title VI of the Civil Rights Act—health care providers who treat patients with public insurance—Medicare, Medicaid and the State Children’s Health Insurance Program (SCHIP)—have an obligation to provide interpreter services to those patients. However, enforcement is subject to judgments about the number of patients with limited-English proficiency affected and the financial burdens imposed on providers. Low payment rates, especially in Medicaid and SCHIP, mean that aggressive enforcement could hinder physicians’ willingness to treat these patients.
Therefore, it is not surprising that physicians working in hospital and other institutional settings were more likely to have interpreter services available than physicians in solo or group practices. As of 2008, all 50 states had laws governing language services in health care settings.13 However, these laws vary by state, languages and/or conditions covered, provider setting, and level of enforcement. Moreover, only some states provide reimbursement for interpreters under Medicaid and SCHIP, and often these states rank among those with the fewest residents with limited-English proficiency.
Even when interpreters are available, the benefit to the patient can be uncertain. Providers often rely on patients’ relatives, untrained bilingual staff or other ad-hoc interpreters. The fact that the provision of interpretation services shows little relationship to physician reports of difficulties with language and cultural barriers raises questions of effectiveness. Little policy attention has been given to clarifying the legal framework governing interpreter services and establishing uniform standards for interpreter services. However, in September 2009, a new group, the Certification Commission for Healthcare Interpreters, was formed to establish national certification for health care interpreters, and the National Council on Interpreting in Health Care is developing national training standards for interpreters."
Many private insurers’ physician directories list languages spoken by participating physicians, and the public sector might consider similar steps to direct patients to physicians who speak their language or offer appropriate interpreter services. Moreover, policy makers likely will need to consider additional subsidies to support interpretation services.
The challenges physicians face in providing quality health care to all of their patients will keep mounting as the U.S. population continues to diversify and the minority population grows. Although disparities can stem from factors beyond the physician-patient encounter, the ability of physicians to communicate effectively with patients and understand their cultural and social context is important in caring for a diverse patient population.
Back to Top
Notes
| 1. | Smedley, Brian D., Adrienne Y. Stith and Alan R. Nelson (eds.) Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, Institute of Medicine (2003). |
| 2. | These measures were included in the 2003 Institute of Medicine (IOM) report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, which identified physician bias, stereotyping and uncertainty on the part of providers as factors influencing disparities. Similar recommendations are contained in National Quality Forum guidelines. See http://www.qualityforum.org/Topics/Disparities.aspx. |
| 3. | These estimates come from the 2008 American Community Survey 1-Year Estimates published by the U.S. Census Bureau. The full table can be found on the Census Bureau Web site at Table S1601, Language Spoken at Home. |
| 4. | Use of interpreters in clinical encounters, especially those who are professionally trained, has been associated with higher provider and patient satisfaction (Carrasquillo, Olveen, et al., “Impact of Language Barriers on Patient Satisfaction in and Emergency Department,” Journal of Internal Medicine, Vol. 14, No. 2 (February 1999)) and improved health outcomes via reductions in errors and enhanced patient comprehension and utilization (Jacobs, Elizabeth A., et al., “Overcoming Language Barriers in Health Care: Costs and Benefits of Interpreter Services,” American Journal of Public Health, Vol. 95, No. 5 (May 2004)). Conversely, language barriers are commonly associated with lack of a usual source of care, lower health service utilization, poor adherence to and misunderstanding of treatment and follow-up regimens, lower satisfaction, and higher incidence of medical complications (Karliner, Leah S., et al., “Do Professional Interpreters Improve Clinical Care for Patients with Limited English Proficiency? A Systematic Review of the Literature,” Health Services Research, Vol. 42, No. 2 (April 2007)). |
| 5. | The relationship between the percentage of patients with whom physicians have difficulty communicating and the number of languages for which their main practice provides translation services is only slightly attenuated after adjusting for the percentage of Latinos, Asians and Native Americans who are treated. |
| 6. | U.S. Department of Health and Human Services, Healthy People 2010: Understanding and Improving Health (November 2000). |
| 7. | 7. Baker, David W., et al., “Health Literacy and Mortality Among Elderly Persons,” Archives of Internal Medicine, Vol. 167, No. 14 (July 2007). |
| 8. | Roter, Debra L., et al., “Effectiveness of Interventions to Improve Patient Compliance: A Meta-Analysis,” Medical Care, Vol. 36, No. 8 (August 1998). |
| 9. | Roughly three-quarters of physicians are in practices that treat patients with at least one of the four focal chronic conditions. Ninety percent of primary care physicians are in practices that treat all of the four conditions. |
| 10. | Betancourt, Joseph R., et al., “Defining Cultural Competence: A Practical Framework for Addressing Racial/Ethnic Disparities in Health and Health Care,” Public Health Reports, Vol. 118 (July/August 2003). |
| 11. | All six measures are not relevant to all physicians. For example, interpreter services are not relevant to the 3.5 percent of physicians with no non-English speaking patients. Moreover, we are not able to assess whether the quarter of physicians in practices that do not treat any of the four major chronic conditions provide patient information materials in languages other than English for conditions they do treat. See Table 2 notes for more information. |
| 12. | In addition to practice type and percentage of minority patients, other physician and practice characteristics are associated with adoption of practices to reduce racial and ethnic disparities. Minority—black and Hispanic—physicians are more likely to implement each of the tools than white, non-Hispanic physicians. With the exception of receiving patient demographic reports, the same is true for physicians practicing in large urban areas relative to rural areas. Across specialties, primary care physicians and medical specialists were more likely than surgeons to provide patient-education materials in languages other than English, have received minority health training, have IT available to obtain patients’ preferred languages, and receive quality reports according to race or ethnicity, while surgeons were more likely to provide interpreters. |
| 13. | Au, Melanie, Erin Fries Taylor and Marsha Gold, Improving Access to Language Services in Health Care: A Look at National and State Efforts, Policy Brief, Mathematica Policy Research, Washington, D.C. (April 2009). |
Back to Top
Data Source
This Issue Brief presents findings from the HSC 2008 Health Tracking Physician Survey, a nationally representative mail survey of U.S. physicians. The sample of physicians was drawn from the American Medical Association master file and included active, nonfederal, office- and hospital-based physicians providing at least 20 hours per week of direct patient care. Residents and fellows were excluded. The survey includes responses from more than 4,700 physicians and had a 62 percent response rate. Estimates from this survey should not be compared to estimates from HSC’s previous Community Tracking Study Physician Surveys because of changes in survey administration mode from telephone to mail, question wording, skip patterns, sample structure and population represented. More detailed information on survey content and methodology can be found at www.hschange.org.
Funding Acknowledgement:
This research was funded by the Robert Wood Johnson Foundation.
Back to Top
RESEARCH BRIEFS are published by the Center for Studying Health System
Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org