
Suburban Poverty and the Health Care Safety Net
HSC Research Brief No. 13
July 2009
Laurie E. Felland, Johanna Lauer, Peter J. Cunningham
Although suburban poverty has increased in the past decade, the availability
of health care services for low-income and uninsured people in the suburbs has
not kept pace. According to a new study by the Center for Studying Health System
Change (HSC) of five communities—Boston, Cleveland, Indianapolis, Miami
and Seattle—low-income people living in suburban areas face significant
challenges accessing care because of inadequate transportation, language barriers
and lack of awareness of health care options. Low-income people often rely on
suburban hospital emergency departments (EDs) and urban safety net hospitals
and health centers. Some urban providers are feeling the strain of caring for
increasing numbers of patients from both the city and the suburbs. Both urban
and suburban providers are attempting to redirect patients to more appropriate
care near where they live by expanding primary care capacity, improving access
to specialists, reducing transportation challenges, and generating revenues
to support safety net services. Efforts to improve safety net services in suburban
areas are hampered by greater geographic dispersion of the suburban poor and
jurisdictional issues in funding safety net services. To improve the suburban
safety net, policy makers may want to consider flexible and targeted approaches
to providing care, regional collaboration to share resources, and geographic
pockets of need when allocating resources for community health centers and other
safety net services and facilities.
- Increased Suburban Poverty
- Limited Suburban Safety Net
- Suburban Access Barriers
- Urban Safety Nets Feel Strain
- Stretching and Improving the Suburban Safety Net
- Broad Community Strategies Lacking
- Policy Implications
- Notes
- Community Maps
- Data Source and Funding Acknowledgement
Increased Suburban Poverty
![]() he considerable movement of affluent and working-class
families into suburban areas throughout the latter half of the 20th century,
which led to increased concentrations of low-income people in the urban core,
has halted and even reversed in recent years. While poverty rates in central
city areas have followed national trends—declining during the 1990s but
edging up since 20001—poverty rates in suburban areas
have increased steadily since 1990.2 Because of more rapid
population growth and increasing poverty rates in suburban areas compared with
central cities, suburban areas accounted for more than half of all poor people
in major metropolitan areas by 2005, compared with 46 percent in 1990.3
he considerable movement of affluent and working-class
families into suburban areas throughout the latter half of the 20th century,
which led to increased concentrations of low-income people in the urban core,
has halted and even reversed in recent years. While poverty rates in central
city areas have followed national trends—declining during the 1990s but
edging up since 20001—poverty rates in suburban areas
have increased steadily since 1990.2 Because of more rapid
population growth and increasing poverty rates in suburban areas compared with
central cities, suburban areas accounted for more than half of all poor people
in major metropolitan areas by 2005, compared with 46 percent in 1990.3
In addition, suburbs have become more culturally and ethnically diverse. By 2000, more than a quarter of suburban residents were non-white, 10 percent were foreign-born and one in six suburban residents spoke a language other than English.4 Reasons for rising suburban poverty include: affluent professionals’ renewed interest in living in central cities, which can increase housing costs beyond what poor families can afford;5 decentralization of low-income housing; relocation or expansion of low-wage jobs to suburban areas;6 and migration of many middle-class families away from older, inner-ring suburbs to more affluent, outer-ring, or exurban, areas.7
Despite the increase in suburban poverty, development of social service programs to assist the poor has lagged. One study found that publicly financed or subsidized services, such as food assistance, job training and adult education, are much less available in suburban areas with increasing poverty than in central-city areas.8 Similar gaps have been identified for some health care services, such as mental health, substance abuse treatment9 and hospital care. Poor suburban areas have less hospital capacity than wealthier suburbs, and the poorest suburbs saw the greatest decline in the number of hospitals among urban and suburban areas between 1996 and 2002.10
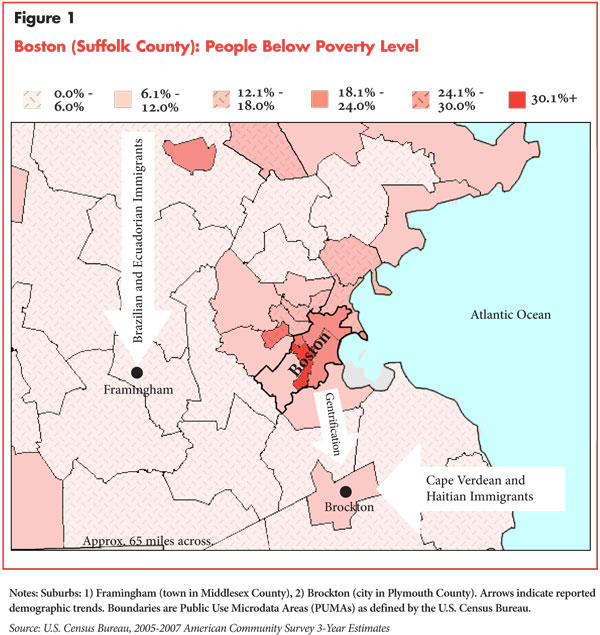
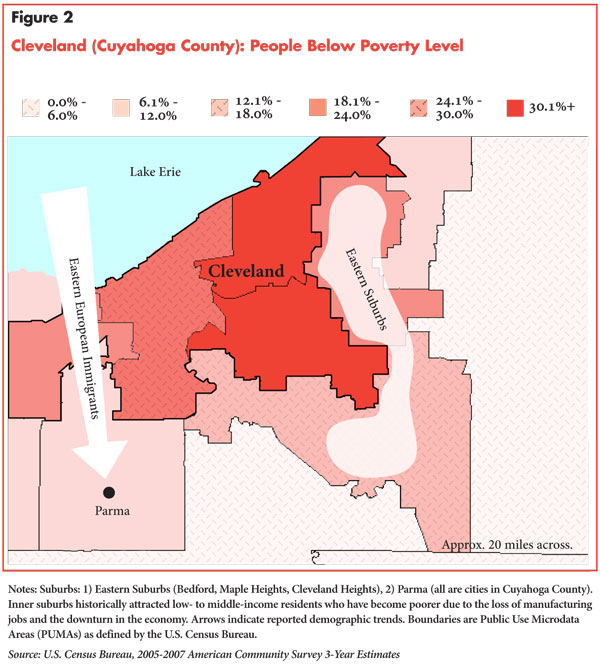
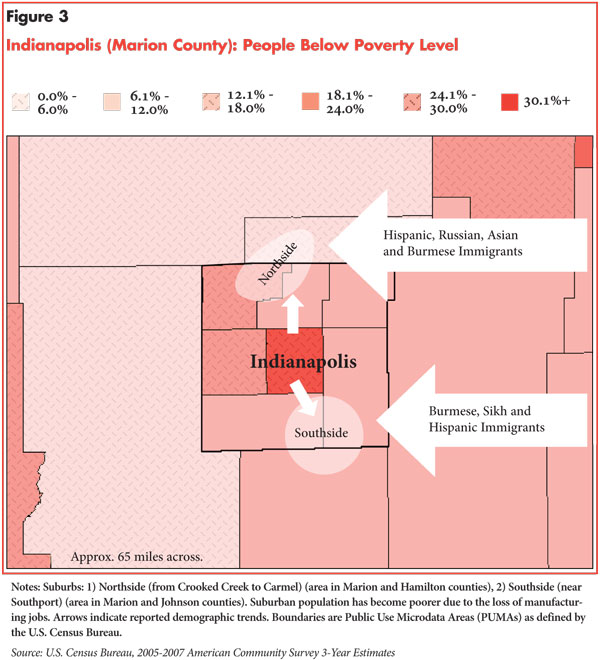
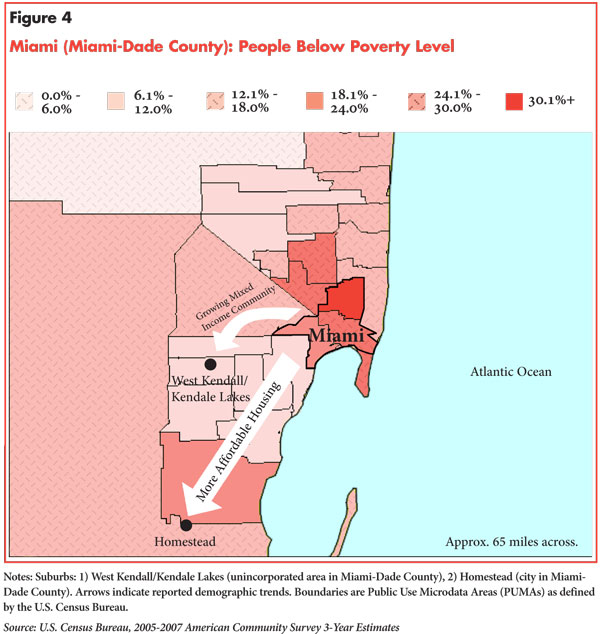
This study provides a community-level examination of the suburban safety net: the health care providers and services available to low-income people in the suburbs. It is not limited to individuals strictly defined as poor, or those with incomes at or below the federal poverty level, or $22,050 for a family of four in 2009, because the income level of the population served by safety net providers is broader—usually at least two times the federal poverty level. The study examined five metropolitan areas—Boston, Cleveland, Indianapolis, Miami and Seattle—including two suburban areas in each with rising poverty rates (see Data Source). All five areas have relatively extensive safety nets in their central-city areas that benefit from longstanding public financial support.
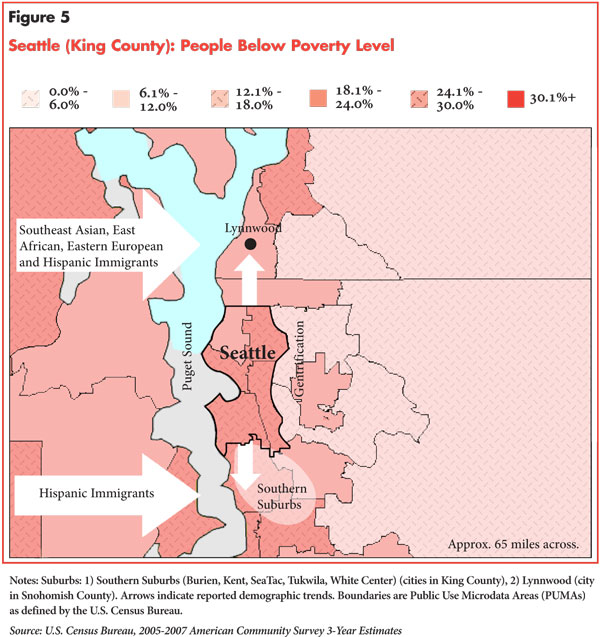
Although the five communities are not representative of all metropolitan areas, interviews with health care providers in these areas offer important insights into the challenges of providing care to low-income people in suburban areas and the interaction between urban and suburban safety nets. The five areas also differ in terms of demographic characteristics of the low-income population, proximity of suburbs to central cities, and the degree to which poverty in the suburbs has been longstanding or is a more recent trend (see maps).
Back to Top
Limited Suburban Safety Net
![]() cross the five communities, respondents reported that urban areas
provide better access to free or low-cost care for low-income people than suburban
areas. Higher levels and concentration of low-income and uninsured people in
urban areas have led to more capacity and choice of providers than typically
found in the suburbs. Safety net services in the central city of the five communities
generally are organized around a large teaching hospital (public or private
not-for-profit), supplemented by multiple outpatient primary care facilities,
including not-for-profit community health centers (CHCs), religiously affiliated
or other free clinics, and, in some sites, local health departments.
cross the five communities, respondents reported that urban areas
provide better access to free or low-cost care for low-income people than suburban
areas. Higher levels and concentration of low-income and uninsured people in
urban areas have led to more capacity and choice of providers than typically
found in the suburbs. Safety net services in the central city of the five communities
generally are organized around a large teaching hospital (public or private
not-for-profit), supplemented by multiple outpatient primary care facilities,
including not-for-profit community health centers (CHCs), religiously affiliated
or other free clinics, and, in some sites, local health departments.
In the suburbs studied, few had a public safety net hospital. Instead a local hospital (typically not-for-profit) generally assumed that role either by mission or default. Some hospitals’ safety net roles are largely limited to their emergency departments, and they may limit access to other services. Other hospitals offer a broader range of services to low-income people.
For example, the suburban areas of Indianapolis and Miami have religiously affiliated hospitals with missions to serve people regardless of their ability to pay for care. However, suburban hospitals do not necessarily focus on serving low-income people. Access reportedly is more difficult at for-profit hospitals, and some urban hospital systems expanded into suburban areas to capitalize on higher-income populations and likely did not plan on encountering more low-income patients. In one suburban area studied—Beech Grove in suburban Indianapolis—the hospital playing a key safety net role is closing as the St. Francis Hospital system consolidates facilities in an area farther from the city center. However, there are plans to retain some outpatient health center services in Beech Grove.
In all five communities, low-income suburban residents reportedly have difficulty accessing preventive, primary and specialty care. Although the suburban areas studied typically have a plentiful supply of private-physician practices, respondents reported that it is difficult—even more so than in urban areas—to find physicians willing to treat uninsured patients and those covered by Medicaid, which provides comparatively lower reimbursement rates than commercial payers and Medicare. Finding private specialty physicians to serve uninsured and Medicaid patients is especially challenging. Health departments in these suburban counties are often quite small and rarely offer direct health care services. The suburbs examined typically have at most one CHC organization and small free clinics and/or hospital outpatient clinics—operated by either suburban hospitals or urban safety net hospitals. CHCs and suburban hospitals typically provide limited specialty, dental and mental health services, and suburban residents often rely on the main urban safety net hospitals, especially for highly specialized care. Similarly, county-operated and other mental health or substance abuse services are more often located in urban areas.
Because of the lack of available, timely care in the community, suburban hospital emergency departments have become a major source of routine and specialty care for low-income people, perhaps even more so than for those living in the central city. Homestead Hospital outside of Miami saw a significant increase in ED volume in the last few years, which respondents attributed to limited availability of primary care for uninsured and Medicaid patients in the community, as well as convenience factors, such as the hospital’s new location close to a highway and around-the-clock care. The experience of a suburban Seattle community hospital was similar: “A lot of people show up in our ED because they can’t get care in the community. There are no free clinics. We don’t have the kind of set up they have in Seattle.”
Rising demand in the last five years has placed financial pressure on many suburban hospitals and health centers. Increased charity care costs at Stevens Hospital in suburban Seattle have contributed to financial challenges and delays in facility improvements. And St. Francis Community Health Center in suburban Indianapolis has seen a 35 percent increase in visits over the last five years, overwhelming the limited capacity of the center. Some suburban providers reported that much of the increased demand is from the so-called new poor—higher-income people who have lost their jobs and health insurance. Additionally, respondents reported many suburban working poor: people who hold low-wage jobs that do not offer health insurance and who make too much to qualify for Medicaid or other subsidized insurance.
Yet, because suburban providers typically serve smaller proportions of low-income people than their urban counterparts, they are less likely to receive public funds to support these services. They compete for broad hospital and health center funding pools and do not receive separate geographic designations and funding streams like rural hospitals and rural health centers. Some suburban hospitals in the five communities receive Medicaid disproportionate share hospital (DSH) funding—particularly those in suburbs with longer-standing low-income populations, such as Brockton, Mass.—but few receive funding from other state or local sources to support care for the uninsured. Suburbs in separate counties from the city center typically do not allocate local revenues (e.g., property or sales tax revenues) to support the health care safety net, and suburbs in the same jurisdiction typically compete with urban safety providers for available dollars. In Massachusetts, for instance, safety net providers are heavily reliant on federal and state dollars because of a lack of municipal or county funding.
While there are federally qualified health centers (FQHCs) in some suburban areas, obtaining federal designation and funding is a challenge. Community Health of South Dade, an FQHC in suburban Miami, attempted to build a new site in the Kendall community but was unable to obtain a public or private grant because, although there are pockets of poverty, the Census tract as a whole does not indicate sufficient need. As a result, many suburban providers rely on private grants and philanthropy to support their safety net role.
Back to Top
Suburban Access Barriers
![]() iving in the suburbs presents a number of additional challenges that
hinder low-income people’s ability to get timely, appropriate health care
services, including:
iving in the suburbs presents a number of additional challenges that
hinder low-income people’s ability to get timely, appropriate health care
services, including:
- limited transportation options;
- insufficient cultural and linguistic competency of providers;
- lack of awareness of available services; and
- community resistance, albeit limited.
Transportation: Almost all respondents identified transportation as a significant barrier to obtaining health care services in the suburbs, where residences and providers are more dispersed and people must travel farther for care. Many low-income people do not own cars and must rely on family or friends to drive them or on public transportation—options that often are unreliable or insufficient. Buses and trains do not always serve suburban areas, and those that do are typically organized using a hub-and-spoke model, which offer transportation from the suburbs to the city but not within or among suburban areas. A CHC representative in suburban Indianapolis remarked, “If it [a procedure or test] can’t be done [at the closest hospital to the CHC], you can tell the patient’s stress level rises.” Although Medicaid provides some transportation assistance and FQHCs are required to provide or contract for transportation services, the requirements are limited to the lowest cost transportation option (usually buses), which might not meet an individual patient’s needs.
Transportation barriers reportedly increased reliance on emergency departments for routine and follow-up care and tests. Since EDs offer around-the-clock care without an appointment, a person can seek care when they are able to obtain transportation. Also, EDs tend to be more accessible by public transportation than other providers. Yet, a few EDs in the five communities have observed increased use of ambulances over the last few years, which is the most expensive mode of transport.
Cultural and Linguistic Competency: Although the suburban areas studied have experienced influxes of immigrants—Hispanic populations as well as people from various other regions—suburban health care providers typically lag their urban counterparts in offering interpreter language services and providing immigrants and minority groups culturally competent care—care that acknowledges an immigrant or other minority group’s beliefs and preferences toward medical consultations and interventions.
As an urban Boston safety net hospital executive explained, “We offer 18 languages onsite 24 hours a day. There’s no other hospital in the state with that much cultural and linguistic competency.” Suburban providers—for example, those in Indianapolis trying to meet the language and cultural needs of recent refugees from Myanmar (formerly Burma)—face challenges finding clinicians and other staff with the necessary skills and often do not treat enough patients of certain ethnicities or languages to be able to support needed services. As a suburban Seattle hospital respondent explained, “Our populations are changing so rapidly and expanding. We’re getting more and more people with much more diverse needs, so we’re constantly reassessing what kind of services we’re providing.”
Lack of Awareness: Many low-income people, especially those who have recently lost their health insurance or jobs, reportedly are unaware of available services in the suburbs or may view facilities like community health centers as only for the poorest uninsured and Medicaid patients.
Some of the first county clinics in suburban Indianapolis struggled to attract enough patients, particularly those above the poverty level who were not accustomed to using safety net providers. A community assessment informed St. Vincent Indianapolis Hospital that low-income people were often unaware of their services and that language issues were a key barrier. In response, the hospital has expanded its Web site and developed materials in multiple languages. However, finding ways to successfully publicize their services remains a challenge for suburban safety net providers. According to a suburban Cleveland CHC director, “We’ve done studies on what brings patients to us. Word of mouth is number one: family and friends encourage them to come to us.” Even if low-income people are aware of safety net providers, they may not know about support services, such as transportation assistance, available to help them get care.
Local Resistance: Most respondents had not observed resistance by suburban residents to establish services for low-income people, although Framingham, Mass., represents an isolated but significant example of community opposition. In 2003, residents fought development of an FQHC to provide primary care primarily for Brazilian immigrants who otherwise were traveling to Boston or Worcester (over an hour away) to seek health care. Residents argued that the center would attract more poor people to the town and hinder business development.
As one respondent explained, “[Residents] saw their town develop and now
they see [the poverty] they tried to escape from in Boston in their backyards.”
Although the local planning board initially rejected the proposal for the health
center, three small sites were built that did not require board permission,
and a later lawsuit allowed the construction of a larger freestanding site.
Respondents said the feared influx of low-income people from elsewhere had not
materialized.
Urban Safety Nets Feel Strain
![]() ome urban safety net providers in the five communities reported an
increase—tracked by patients’ zip codes—in suburban patients,
which places additional strain on already busy and financially strapped urban
providers. Often, suburban patients seeking care from urban safety net providers
need difficult-to-access services, such as specialty, dental and mental health
care. Approximately 16 percent of patients at Codman Square Community Health
Center in Boston live in the suburbs, compared with about 6 percent of patients
10 years ago. Although some urban safety net hospitals reported little demand
from suburban patients, none reported an overall decline in urban and suburban
volumes that would indicate a net shift in low-income patients and demand for
care to outlying areas.
ome urban safety net providers in the five communities reported an
increase—tracked by patients’ zip codes—in suburban patients,
which places additional strain on already busy and financially strapped urban
providers. Often, suburban patients seeking care from urban safety net providers
need difficult-to-access services, such as specialty, dental and mental health
care. Approximately 16 percent of patients at Codman Square Community Health
Center in Boston live in the suburbs, compared with about 6 percent of patients
10 years ago. Although some urban safety net hospitals reported little demand
from suburban patients, none reported an overall decline in urban and suburban
volumes that would indicate a net shift in low-income patients and demand for
care to outlying areas.
Urban county hospitals in Cleveland, Seattle and Indianapolis have identified more low-income people coming from outlying areas for care. MetroHealth System in Cleveland, which is reportedly relatively accessible from the suburbs, receives significant county funding to support indigent care and offers a sliding-fee scale for low-income patients. Consequently, many suburban low-income people both in Cuyahoga County (Cleveland) and surrounding counties seek care there or are referred. A suburban Cleveland hospital respondent said, “If someone [a low-income patient] became expensive and needed specialist services, [the county hospital] is where they [suburban providers] effectively shift everyone to.”
Because many of the suburban patients directed to these urban county hospitals are from different counties, the urban hospitals are questioning the lack of other jurisdictions’ support for safety net services. They argue that counties should subsidize their own providers to treat these patients, that not-for-profit hospitals are obligated to provide services to the community in exchange for their tax-exempt status, and that some referrals or transfers are not best for the patient.
In response, MetroHealth has implemented a policy to no longer treat non-emergent patients from outside of Cuyahoga County, while the county hospital in Seattle, Harborview Medical Center, has collaborated with the state hospital association and suburban hospitals to limit referrals of low-income suburban patients. According to a Seattle respondent, “As the safety net hospital for our county, [Harborview] has quickly become the safety net hospital for the entire state. We’ve really had to push back. It wasn’t uncommon to get patients from 100 miles away with a nice letter from their physician saying the person lost their insurance and they can’t care for the patient anymore.”
Back to Top
Stretching and Improving the Suburban Safety Net
![]() oth urban and suburban providers are attempting to improve the availability
of health care services for low-income suburban residents. The motivation is
twofold—an organizational mission or desire to improve access and a desire
to encourage appropriate use of services. Strategies include:
oth urban and suburban providers are attempting to improve the availability
of health care services for low-income suburban residents. The motivation is
twofold—an organizational mission or desire to improve access and a desire
to encourage appropriate use of services. Strategies include:
- expanding primary care capacity;
- decreasing reliance on emergency departments;
- improving access to specialists;
- reducing transportation challenges; and
- generating revenue by pursuing higher-income patients.
Expand primary care capacity. Of the five communities, only in Miami has the main safety net hospital—Jackson Health System—added new hospitals in suburban areas over the last few years. Rather, urban and suburban hospitals, along with health centers, have focused on increasing primary care capacity. Many suburban CHCs have expanded their existing physical space, staff and clinic hours to include evening and weekend appointments, which are particularly helpful for working, low-income patients who commute to the city. Indeed, respondents surmised that people tend to seek health care near their home rather than near their workplace. Health centers have also added specific services, including dental and mental health care, and are attempting to recruit clinicians and interpreters who match the language and ethnicity of many of their patients.
Some urban and suburban CHCs also are building new facilities. Sea Mar Community Health Centers, an FQHC in the Seattle area, recently added two new facilities in the southern suburbs. Some new clinics target particular racial and ethnic minorities. Wishard Health Services in Indianapolis has collaborated with St. Vincent’s Indianapolis Hospital to develop a clinic for the growing suburban Hispanic population. Wishard operates and staffs the Pecar Health Center with Spanish speakers, while St. Vincent’s provides in-kind support, including services and products (e.g., cribs and car seats) that encourage women to obtain prenatal care.
However, CHCs often focus their expansions in somewhat limited geographic areas to avoid being spread too thin, competing with other health centers, or being unable to cover costs if they are located in areas without a large Medicaid population base (for which FQHCs receive enhanced reimbursement).
Decrease reliance on emergency departments. Although many suburban hospitals are expanding ED capacity to meet immediate demand—both Brockton Hospital in suburban Boston and Highline Medical Center in suburban Seattle are doubling the size of their EDs—they also are trying to enhance primary care access and reduce pressure on their EDs. Hospitals in suburban Indianapolis and Boston have built primary care clinics, and Brockton Hospital acquired a primary care physician practice to provide follow-up care to the uninsured. A number of hospitals support CHCs and free clinics by providing direct funding, space, supplies, services (such as lab and radiology) and staff (even grant-writing support and management in some cases) instead of assuming the capital and operating expense that would be required to open their own clinics.
Part of the strategy to redirect patients from the ED involves working with providers and patients to increase awareness of primary care options. St. Francis Neighborhood Health Center in suburban Indianapolis found that private-practice physicians and ED physicians were treating non-urgent patients multiple times before learning they could refer them to the CHC. In the Miami suburbs, Homestead Hospital and Community Health of South Dade work collaboratively to address the issue: the hospital gave a grant to the CHC to offer after-hours appointment availability and provides brochures in the ED to inform patients about the availability of follow-up care at the health center.
Improve access to specialists. Some urban safety net hospitals are attempting to station specialist physicians at suburban hospitals and health centers on a regular basis to improve access and reduce the no-show appointment rate. As a representative from Jackson Health System in Miami explained, “In specialty clinics, there’s still a no-show rate greater than 30 percent. So we’re always looking at ways to improve compliance. And sometimes it’s a matter of taking the care to the people, or being more flexible and adjusting our hours and days of operation.” Jackson also is employing more doctors to treat uninsured people under its charity care policy. Similarly, some suburban health centers are partnering with urban medical and dental schools for training opportunities for students who in exchange treat patients at the health center.
In some communities, safety net providers are encouraging physicians, especially specialists, in suburban areas to volunteer to treat a set number of uninsured patients in their own practices through programs typically operated by local medical societies, commonly referred to as Project Access programs. Harborview Medical Center in Seattle has worked with suburban private physicians in this way as part of its effort to shift the care for low-income patients back to the communities where they live.
Reduce transportation challenges. Providers are attempting to add more reliable and direct transportation options for patients. Health centers in suburban Miami, for example, offer a van service between their facilities and the Jackson Health System. MetroWest Medical Center in Framingham, Mass., worked with a community bus line to improve access to and from its hospital.
In addition, provider and community efforts to bring certain services directly to low-income neighborhoods have emerged, especially in Miami and Seattle, which are relatively large geographic areas with pockets of low-income people. In the Miami-Dade County area, Jackson Health System, the health department and CHCs operate mobile services for medical screenings and dental services. The King County (Seattle) Health Department is using mobile vans to serve the homeless. King County also is developing school-based clinics in suburban schools, and Miami-Dade County has an extensive initiative to add school-based health services in all of its schools—urban and suburban—funded through a property tax assessment for children’s services passed by voters in 2002.
Generate revenues by pursuing higher-income patients. Since poverty
and wealth often co-exist in suburban areas, some urban safety net hospitals’
addition of services in suburban areas reflect a dual strategy to expand access
to low-income people while also attracting higher-income, well-insured patients,
who help subsidize care for low-income patients. This was one motivation for
MetroHealth in Cleveland to add suburban primary care centers and for Jackson
Health System in Miami to expand hospital services into suburban areas.
Back to Top
Broad Community Strategies Lacking
![]() part from individual urban and suburban provider efforts to improve
access, there is little broad community or regional collaboration to improve
the suburban safety net in the five communities. Some community planning organizations
and coalitions are examining suburban poverty as part of broader efforts to
improve access to care for low-income people.
part from individual urban and suburban provider efforts to improve
access, there is little broad community or regional collaboration to improve
the suburban safety net in the five communities. Some community planning organizations
and coalitions are examining suburban poverty as part of broader efforts to
improve access to care for low-income people.
For example, the Marion County Health Department in Indianapolis has worked with area hospitals to conduct a needs assessment and to collaborate on community benefit provision to address gaps in care. And CHCs in some sites are collaborating with each other, often through regional CHC consortiums. CHC partnerships are underway in Seattle to expand obstetrical/gynecologic and prenatal care in suburban areas and, in Miami, to create a shared electronic medical record across the area’s CHCs, health department and county hospitals, which could help facilitate and coordinate care between suburban and urban providers.
Back to Top
Policy Implications
![]() ncreasing numbers of low-income people in suburban areas—including
the “new poor” who have lost their jobs and health insurance—signal
a greater need for a suburban health care safety net. In particular, improving
the availability of outpatient primary and specialty care in suburban areas
may decrease the use of costly emergency departments for non-urgent needs or
urgent situations that could have been avoided through more timely access to
care.
ncreasing numbers of low-income people in suburban areas—including
the “new poor” who have lost their jobs and health insurance—signal
a greater need for a suburban health care safety net. In particular, improving
the availability of outpatient primary and specialty care in suburban areas
may decrease the use of costly emergency departments for non-urgent needs or
urgent situations that could have been avoided through more timely access to
care.
However, because suburban poverty is often dispersed, building a comprehensive system that stands apart from the urban safety net may not be practical or cost-effective in many suburbs, especially because low-income groups will continue to migrate to new areas. Instead, state and local governments and community groups could improve access to appropriate care by subsidizing services through existing providers; supporting more targeted and flexible approaches to providing services where people live, for example, through school-based clinics and mobile vans; and addressing transportation needs. Further, as low-income people are often largely invisible in suburban areas, broader efforts to boost awareness of available services could help improve access. The suburban safety net could also benefit from urban and suburban policy maker attention to how funding is allocated and other barriers to expanding access across county lines and other jurisdictions. Formation of regional alliances could help urban and suburban areas share resources and create networks of care across jurisdictions.11
Although national health reform could improve access to insurance coverage and care for low-income people regardless of where they live, designated safety net providers will likely remain essential in areas with large concentrations of low-income people. Such providers readily accept patients with public insurance and have expertise in serving vulnerable groups, including offering translation services for limited-English-speaking patients, culturally competent care, transportation and other support services.
Indeed, the federal government signaled strong support for continued community
health center funding in the American Recovery and Reinvestment Act of 2009,
including grants for 126 new health center sites and to support increased demand
for services at existing FQHCs. As federal, state and local policy makers debate
future funding for safety net facilities, they could consider ways to fine tune
how medically underserved areas and populations are identified and selected
for federal funding to ensure that large pockets of low-income people in otherwise
higher-income areas are not overlooked.
Back to Top
Notes
Back to Top
Community Maps
Data Source
The five study communities—Boston, Cleveland, Indianapolis, Miami and
Seattle—were selected from the 12 nationally representative Community Tracking
Study (CTS) sites. Using a combination of data from the 1990 and 2000 Census
and the 2006 American Community Survey, maps were created for each of the 12
CTS sites, illustrating the percentage of the population below the federal poverty
level, with the help of Social Explorer® software (available at www.socialexplorer.com)
and the U.S. Census Bureau Web site. From these maps and data collected during
the 2007 CTS site visits, five sites were selected that appeared to have large
or growing areas of suburban poverty. From a demographic data perspective, there
is no formal definition of a suburb; two areas within each metropolitan statistical
area but outside of the center city were identified that appeared to have higher
or growing rates of poverty. These selections were confirmed qualitatively through
a brief interview with a health care expert in each community. Between July
and December 2008, a total of 60 telephone interviews were conducted in the
five communities with representatives of urban and suburban hospitals that play
a safety net role, community health centers and clinics, local health departments,
and other knowledgeable observers. A two-person research team conducted each
interview, and notes were transcribed and jointly reviewed for quality and validation
purposes. The interview responses were coded and analyzed using Atlas.ti, a
qualitative software tool.
Funding Acknowledgement:
This research was funded by the Robert Wood Johnson Foundation.
Back to Top
RESEARCH BRIEFS are published by the Center for Studying Health System
Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org