
Aging Plays Limited Role in Health Care Cost Trends
Data Bulletin No. 23
September 2002
Bradley C. Strunk, Paul B. Ginsburg
![]() espite widespread belief to the contrary, aging baby boomers
are not a major driver of rapidly rising health care costs for Americans under
age 65, according to new findings from the Center for Studying Health System Change
(HSC). In 2001, population aging contributed an estimated 0.7 percentage points,
or less than 10 percent of the total increase in per capita health care spending
for people under 65 (see Figure 1). The trend in per capita
health care spending determines the long-term trend in private health insurance
premiums for people under 65.
espite widespread belief to the contrary, aging baby boomers
are not a major driver of rapidly rising health care costs for Americans under
age 65, according to new findings from the Center for Studying Health System Change
(HSC). In 2001, population aging contributed an estimated 0.7 percentage points,
or less than 10 percent of the total increase in per capita health care spending
for people under 65 (see Figure 1). The trend in per capita
health care spending determines the long-term trend in private health insurance
premiums for people under 65.
Figure 1
Effect of U.S. Population Aging on Health Care Costs
(Annual Percentage Change)
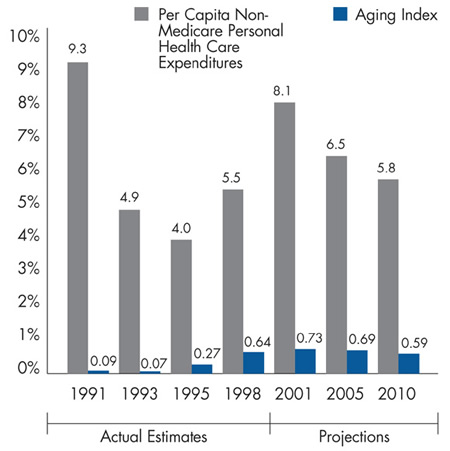
Sources: Aging Index—authors’ calculations using data from the 1996 and 1997 Medical Expenditures Panel Survey and U.S. resident population estimates and projections of the under-65 population from the U.S. Census Bureau; Per Capita Non-Medicare Personal Health Care Expenditures—from the National Health Accounts, maintained by the Centers for Medicare and Medicaid Services
Explaining the Misconception
![]() ealth spending increases with age because older people tend
to have more medical needs than younger people. Thus, average health spending
per person for the population as a whole will rise as the average age of the population
increases. With the leading edge of the baby boom generation now in its mid-50s,
policy makers increasingly have focused on the relationship between aging and
rising health care costs. The magnitude of aging’s influence on costs depends
on how steeply spending per person increases with age and the pace at which the
population ages.
ealth spending increases with age because older people tend
to have more medical needs than younger people. Thus, average health spending
per person for the population as a whole will rise as the average age of the population
increases. With the leading edge of the baby boom generation now in its mid-50s,
policy makers increasingly have focused on the relationship between aging and
rising health care costs. The magnitude of aging’s influence on costs depends
on how steeply spending per person increases with age and the pace at which the
population ages.
Annual per capita health spending increases by about $74 on average (2001 dollars) for each additional year in age between 18 and 64, although spending starts rising more rapidly after age 50—about $152 for each additional year in age between 50 and 64. The average age of Americans younger than 65 is increasing about 0.13 years annually.
So differences in spending by age are not large enough and the U.S. population is not aging quickly enough to make aging a major cost driver for the under-65 population. For certain categories of health care services, such as cardiovascular services, aging may be a more important factor than it is for all types of services combined.
Aging’s Past and Future Effect on Costs
![]() opulation aging contributes more today
to trends in health care spending for
people under 65 than it did in the early
1990s. In fact, from 1990 to 1995, spending
increases due to aging ranged from 0.1
percent to 0.3 percent because most
baby boomers had not yet reached 50.
opulation aging contributes more today
to trends in health care spending for
people under 65 than it did in the early
1990s. In fact, from 1990 to 1995, spending
increases due to aging ranged from 0.1
percent to 0.3 percent because most
baby boomers had not yet reached 50.
Projections through 2010 suggest that the role of aging as a cost driver for the under-65 population will remain limited. For example, in 2005, aging will cause per capita health care spending for people under 65 to increase about 0.7 percent; in 2010, that figure will be 0.6 percent.
In 2011, as the first wave of the estimated 76 million baby boomers turns 65, financing of their care will begin shifting from the employment-based private insurance system to the publicly financed Medicare program. As a result, Medicare spending will begin to increase significantly. However, the larger number of people joining the program, rather than more spending per person, will cause most of the increase. So it’s not primarily the aging of the population as a whole that will drive up Medicare spending; it’s the boomers’ sheer numbers and the shift in the financing of their care from the private to the public sector.
Financing the boomers’ care will severely strain the federal budget, leaving fewer resources for competing spending needs and forcing policy makers to consider tough trade-offs, such as reducing benefits, raising taxes or allowing larger deficits.
Policy Implications
![]() mployers, workers and policy makers
are struggling with the current rapid
growth in private insurance premiums
for people under 65. Increased insurance
costs lead to fewer employers offering
coverage and fewer employees enrolling
in the plans available to them.
mployers, workers and policy makers
are struggling with the current rapid
growth in private insurance premiums
for people under 65. Increased insurance
costs lead to fewer employers offering
coverage and fewer employees enrolling
in the plans available to them.
Since the aging of the population is beyond the control of policy makers and employers, they should gain some peace of mind from the fact that aging is not a major cost driver. Instead, policy makers and employers should look at the more significant factors driving health care spending, including new medical technology, the retreat from tightly managed care, providers of growing ability to demand higher payment rates from health plans and the hospital nursing shortage.
Constructing an Aging Index
![]() his aging index is analogous to a basic quantity index, which measures
changes in expenditures due to changes in quantity alone and are,
therefore, independent of price changes. Data on health care spending
per person by age (analogous to the price in a quantity index calculation)
are from the 1996 and 1997 Medical Expenditures Panel Survey
(MEPS).
his aging index is analogous to a basic quantity index, which measures
changes in expenditures due to changes in quantity alone and are,
therefore, independent of price changes. Data on health care spending
per person by age (analogous to the price in a quantity index calculation)
are from the 1996 and 1997 Medical Expenditures Panel Survey
(MEPS).
Because sample sizes by individual ages are small in the MEPS, we took a number of steps to increase the precision of the estimates of health care spending per person by age. First, for each year of the MEPS, we calculated five-year age range averages for each age (for example, for age 20, we used the weighted mean expenditure for people ages 18 to 22; for age 21, we used the weighted mean expenditure for people ages 19 to 23). Second, we pooled the 1996 and 1997 data by calculating, for each age, the simple average of the 1996 and 1997 estimates obtained in the first step.
Estimates (for 1990-2000) and projections (for 2001-2010) of the U.S. resident population under 65 by age (analogous to the quantity in a quantity index calculation) are from the U.S. Census Bureau.
This Data Bulletin analyzes changes in an aging index that measures the extent to which average health care spending per person under age 65 changes from year to year due solely to the aging of the U.S. population, while holding all other cost drivers constant. See the box for details on how the index was developed.
Data Bulletins are published by the Center for Studying Health System Change (HSC)President: Paul B. Ginsburg
Director of Public Affairs: Richard Sorian
Editor: The Stein Group