
HSC Research Brief No. 12
April 2009
Ann S. O'Malley, Ann Tynan, Genna R. Cohen, Nicole M. Kemper, Matthew M. Davis
Despite calls from numerous organizations and payers to improve coordination of care, there are few published accounts of how care is coordinated in real-world primary care practices. This study by the Center for Studying Health System Change (HSC) documents strategies that a range of physician practices use to coordinate care for their patients. While there was no single recipe for coordination given the variety of patient, physician, practice and market factors, some cross-cutting lessons were identified, such as the value of a commitment to interpersonal continuity of care as a foundation for coordination. Respondents also identified the importance of system support for the standardization of office processes to foster care coordination. While larger practices may have more resources to invest, many of the innovations described could be scaled to smaller practices. Some coordination strategies resulted in improved efficiency over time for practices, but by and large, physician practices currently pursue these efforts at their own expense.
In addition to sharing information on effective strategies among practices, the findings also provide policy makers with a snapshot of the current care coordination landscape and implications for initiatives to improve coordination. Efforts to provide technical support to practices to improve coordination, for example, through medical-home initiatives, need to consider the baseline more typical practices may be starting from and tailor their support to practices ranging widely in size, resources and presence of standardized care processes. If aligned with payment incentives, some of these strategies have the potential to increase quality and satisfaction among patients and providers by helping to move the health care delivery system toward better coordinated care.
![]() espite calls from numerous organizations, patients and
payers about the need to improve and support care coordination, little information
is available about how medical practitioners might better coordinate patient
care, both within and across practices and settings. Coordination of care in
the United States has often been characterized as “poor,”1-4
with negative consequences for patient outcomes5,6
and for provider satisfaction.7 Yet, some physician practices
provide better than average coordination.
espite calls from numerous organizations, patients and
payers about the need to improve and support care coordination, little information
is available about how medical practitioners might better coordinate patient
care, both within and across practices and settings. Coordination of care in
the United States has often been characterized as “poor,”1-4
with negative consequences for patient outcomes5,6
and for provider satisfaction.7 Yet, some physician practices
provide better than average coordination.
In this study, the term coordination of care is used to describe the integration of care across all of a patient’s conditions and health care needs, both within the primary care practice, as well as between the patient’s primary care practice and other providers and settings. Importantly, this definition includes coordination with the patient, family or caregivers.8-10
This study involved in-depth interviews of physicians and national experts to identify current best practices in coordination, challenges and lessons learned (see Table 1 and Data Source). Particular emphasis was placed on identifying respondents in small to medium-sized medical groups because they have received less attention in the literature, even though they constitute the majority of outpatient medical practices and serve the bulk of the population.11 Primary care practices were targeted primarily, since generalists’ training and orientation emphasize well and illness care across a spectrum of acute and chronic conditions and because they often act as the central clinician in coordinating care.8,9 Some specialists were also interviewed to gain their perspectives on coordinating care with primary care generalists; additionally, for a small group of patients with a particularly severe condition dominating their care needs, a specialist might serve as their de facto primary care provider.
The study’s goals were to: 1) inject the experiences of on-the-ground outpatient clinicians and staff facing the reality of everyday practice into discussions of coordination of care, a topic that is receiving increased attention because of medical-home initiatives and other efforts to improve quality and contain costs; 2) share examples of approaches physician practices are using to coordinate care to help facilitate replication; and 3) draw implications for implementation and payment policy around coordination of care. This paper is not an exhaustive review of approaches to coordinating care but rather reflects strategies that real-world practices have implemented and found helpful.

![]() espondents identified numerous challenges to coordination. Challenges from patient and physician behavior were largely believed to be a response to system-level factors.
espondents identified numerous challenges to coordination. Challenges from patient and physician behavior were largely believed to be a response to system-level factors.
Patient Factors: While patients should not be held responsible for system dysfunction, there are particular patient characteristics and behaviors that make coordination more challenging, including the tendency of some patients to self-refer to numerous specialists. Greater coordination required by high-need populations, including people with more economic and social needs and medically complex patients, is also a challenge given the lack of reimbursement for such efforts. Additional challenges include patient noncompliance, risky behaviors and misunderstanding of provider recommendations. The latter is often a result of unclear explanations from providers and, as one respondent noted, the provider failing to “close the loop,”12 by ensuring the patient/family could repeat instructions back to the provider.
Physician Factors: An ongoing challenge to coordination noted by several national experts is the “culture of non-communication and non-ownership of coordination” among providers, described as a direct result of lack of incentives in the reimbursement system for coordination. In addition, some physicians are reluctant to be held accountable for coordinating the care of patients who visit the office infrequently or who disregard medical advice. An additional barrier cited by both primary care physicians and specialists was the quality of consultant notes and referral notes, respectively. Additional challenges at the physician level include lack of emphasis in medical schools and residency around coordination of care. A physician noted that some physicians simply are not aware of how to work within a team to accomplish the numerous coordination tasks required, and that this “requires a paradigm shift.”
System Factors: Respondents were quick to note that existing fee-for-service payment does not reimburse care coordination efforts. Because there are no payments for such activities as following up on referrals or communicating with patients outside of the office, physicians do so at the expense of other, billable activities. A primary care physician captured this common experience, “If you don’t have face-to-face interaction you can’t bill. We can talk to patients, and if you have to eat that cost, you have to eat that cost, but you also have to minimize the time it takes to do it.” Another respondent said, “The more people you see the more money you make—the incentive is volume—so you see how care coordination falls out of the equation.” Although coordinated care would likely lower overall costs to the patient and health care system over time, immediate costs are borne by physicians.
Health plan policies also pose coordination challenges. Plan specialist networks were a barrier to coordination when they were inconsistent with primary care physicians’ referral base. Frequent changes in plan provider networks also pose a challenge—one physician cited an example of a patient whose surgeon was dropped from an insurance network while the patient still needed follow-up care. Similarly, sudden changes in health plan drug formularies can create a spurt of extra work for primary care physicians (PCPs) and disrupt patients’ medication coordination when patients suddenly need to come in for revised prescriptions. Finally, administrative burdens around obtaining approval for referrals were a frequently mentioned challenge.
Almost every primary care practice interviewed links an individual PCP with each patient. The importance of continuity to coordination was summarized by a physician leader as follows: “It’s the persistent focus on continuity that does more to coordinate care than anything else.” To facilitate that interpersonal continuity, the respondent emphasized the importance of retention of physicians and staff, enhanced by a supportive work environment and an attractive benefits package.
The most common strategy used by practices to help coordinate care involved identification of a person within the practice who acted as a referral or care coordinator and shared responsibility for coordination with the PCP. The formalization and responsibilities of that coordinator role varied, as did the clinical training required. Coordinators ranged from “referral specialists” who focused primarily on non-clinical activities, such as obtaining insurance preauthorization for tests, to “care coordinators” who were involved in clinical coordination tasks, patient education and counseling.
Respondent views varied about the level of training required for a coordinator, since behavioral health counseling or care management require advanced training and credentialing. Although some suggested that registered nurses (RNs) or nurse social workers have the ideal background for a care coordinator, the nursing shortage and expense of hiring RNs were a significant limitation for many primary care respondents. Smaller practices emphasized the importance of flexible roles for realizing the efficiencies of delegating coordination activities.
The concept of the primary care team was critical to some of the practices’ coordination efforts. While most teams were somewhat informal, a few practices worked in distinct teamlets or pods. The teamlet strategy consists of a dyad of an independent clinician with a medical assistant(s) or RN.13 Like the use of care coordinators and referral specialists, these structured units strive to maximize efficiency through delegation. A national expert on primary care and coordination noted that teams function optimally when the medical assistants are trained in expanded responsibilities for pre-visit, visit and post-visit functions.14
At Clinica Campesina, a community health center in Colorado, the large administrative and clinical staff is organized into pods—smaller groups with designated patient panels. Assigning patients to a pod increases continuity by keeping patients within a consistent set of care providers. An important element of the pod is the use of “color marking” so that both patients and providers are aware of their mutual relationship and accountability. One physician said, “The thing that made us move [to pods] is that it’s clear to us in multiple ways—outcomes, patient satisfaction—that continuity is the key driver. patients get to know the pod team much better and feel more confident about their care.”
Three practices believed they could coordinate care in part because of a deliberate restriction of their panel size and number of visits per day to “have more time to coordinate care.” While these were not concierge practices—where patients pay the physician an annual fee or retainer for enhanced access—they did care predominantly for insured patients and provided numerous ancillary testing services within their practices.
For practices lacking the economies of scale to support designated care management staff or extensive patient education, there is a strategy of “renting” services they cannot provide in-house. In one example in Connecticut, these services were provided by a physician hospital organization (PHO), the Middlesex Health System, which provides clinical management services to independent physician practices in the community. Patients with particular conditions who are having problems with self-management are referred to this program by their primary care physician. The program works closely with the PCP, and care management is done primarily through face-to-face contact between patients and nurse care managers. Because patients’ physicians refer them to the program, care management is seen “as an extension of care in the physician office rather than an insurance company calling and bugging them.” In the absence of such a resource, a few respondents in other markets leveraged the patient education resources of community hospitals.
Some practices had specialized programs for population-based management to enhance quality and coordination for particular patient groups. For example, a frail elder program in a geriatric practice in Colorado focused intensively on a group of patients with the highest resource needs, using team-based care with a synchronized care plan. The team, comprised of nurses and social workers co-located in and assigned to a primary care practice by the patients’ health plan, makes home visits to reconcile medication and identify unmet needs. The team can access the doctor’s schedule to make urgent appointments and participates in weekly meetings with physicians.
Another example is the use of cluster encounters, where specific days are set aside for patients with a particular condition, such as asthma or diabetes, to come in for maintenance care. Practices using this strategy explained that the structure helps them gain efficiency in tracking care. As one respondent explained, “It is helping us keep track of chronic management, and it helps the nurses focus and keep in the mindset.”
Several practices emphasized the benefits of direct phone access to patients’ personal physician or another familiar member of the primary care team. Respondents in practices emphasizing phone access to physicians noted that it allowed providers to screen problems and guide patients to the appropriate care setting, decreasing the likelihood they would go to the emergency department (ED) or urgent care center and complicate coordination efforts.
A physician whose practice had a designated call-in period described its use in combination with their open-access scheduling system: “We have a call time between 8 and 9 a.m. when patients can talk directly to their primary care physician. We encourage patients who want to come in that day to call during that period so we can set up our day.” Illustrating how this call-in hour enhances coordination, the respondent said, “Patients constantly call us and say ‘I saw Dr. X because the cardiologist sent me to him for my prostate. The cardiologist thought I should have a PSA and a digital exam and said my PSA is high and I should do something about it.’ I’ll say, ‘You’re 92 and I wouldn’t worry about it.’”
Encouraging patient, family and caregiver involvement was emphasized by respondents. A geriatrician explained that “making caregivers feel welcome and acknowledging their role,” can turn caregivers into “invaluable team members” and help keep providers informed of the patient’s needs.
Respondents described efforts to engage patients, their family or caregiver when appropriate, to be more proactive in the coordination of their own care. The three areas of focus for encouraging patient involvement in coordination were patient self-management, medication awareness and keeping one’s PCP informed of care received from other providers.
Self-management: Efforts to encourage patient self-management centered on increasing patient awareness of preventive services and the monitoring of chronic conditions. To engage patients in the coordination of diabetes care, one physician said, “We put a flow sheet and targets for diabetic care into the patient’s hands and say ‘if your A1c isn’t below 7, or you haven’t had an ophthalmology referral lately, come back and ask for it.’” One internist adapted the commonly used pre-appointment questionnaire, adding the questions: “What are you hoping to accomplish today?” and “Is there anything else you would like to work on to improve your health?”
Medication Coordination: Keeping the list of medications and doses up to date, ensuring the patient understands them, and handling refills were time-consuming aspects of coordination mentioned frequently by respondents. For patients seeing multiple specialists or with a recent hospitalization this task increases exponentially. Efforts at medication coordination included printing up-to-date medication lists for patients, medication reconciliation at each visit, ensuring patient awareness of their medications before prescribing refills, and renewal of non-controlled medications at the time of the annual exam for the maximum period allowed when clinically appropriate.
Identifying Self-referrals and Specialist Cross-referrals: In an effort to improve coordination when patients self-refer or are given cross-referrals by one specialist to another, primary care physicians generally took three approaches. First, many discuss with the patient the PCP’s role in coordinating care, encouraging patients to communicate back to them if they see a specialist or have an unexpected ED visit. Second, to encourage other specialists to communicate back to him, one internist said, “I give the patients my card and explain that if they go to any other physicians to have them send me a report and that my office will be the central repository of all information.” Third, some routinely asked patients about care from outside providers and then contacted those specialists for reports.
An internist in solo practice makes home visits to improve coordination: “I started this program to keep people out of the hospital. It’s a comprehensive program across disciplines. I or an assistant visit patients at home when necessary, once or twice a month. We have a phlebotomist, we do echocardiograms, spirometry physical and occupational therapy through nurses, and watch when they are acutely ill. We’ve decreased hospitalization rates, and many patients can now live in their home instead of being transitioned to a skilled-nursing facility.”
Within-office coordination was facilitated by a variety of processes, including role definition and training of staff, daily huddles and team meetings, the use of information technology, and standardization of certain clinical processes.
Several respondents identified the standardization of particular processes as useful to “avoid things slipping through the cracks,” especially at times of provider discontinuity. Standardized processes included achieving consensus among providers in a practice on how patients would be informed of lab results. Another practice implemented a chronic pain medication protocol to avoid narcotics abuse and disruption of patient care when covering physicians were asked to refill a patient’s prescription. Another practice established a feature in its electronic medical record (EMR) to guide the provider through indications for diagnostic testing and referral for low back pain. System support was critical to standardizing processes, as one physician said, “Diabetes can be well managed in primary care as long as the system supports us.”
Planned care visits were also noted to facilitate coordination: “It gets us out of focusing solely on acute-symptom management to also provide comprehensive planned care for chronic illness and prevention. . I’ll plan the next appointment at the end of the current appointment.” Pre-appointment testing was highlighted by a few respondents as particularly helpful, as physicians can then focus the visit on a dialogue with patients about their care rather than fact-finding during the visit and counseling the patient later by phone or mail. Use of a post-appointment order sheet was also felt to streamline subsequent care.
In the half of respondent practices with an EMR, respondents noted that it facilitated within-office coordination because of easy access to information. Given the lack of interoperability, EMRs, however, were described as less useful for between-office coordination, except among physicians in large multi-specialty systems where all providers shared an EMR. In some practices without an EMR, simpler information technology (IT) tools, such as stand-alone disease registries, enabled coordination around chronic disease, preventive services and generation of reminders.
E-mail with patients was cited by one internist as particularly helpful in non-visit communication about “dynamic problems like diabetes,” noting that it “saves people a lot of office visits.” E-mail was also used to help coordinate care for travelling patients, permitting them to attach a photo of a rash or test result for non-emergency problems, rather than having their care fragmented by seeing another provider where access to a trusted practitioner may be unavailable.
To make coordination more manageable and ensure a certain level of quality, several respondents said they limit the size of their referral networks. They believed this strengthened working relationships, particularly when physicians limit their referral base to those who reliably communicate back to the primary care office.
According to one physician, “Even the family doctors I know in big cities where there are literally 30 different cardiology groups, use one or two groups because that’s just human nature—you need working relationships.” Moreover, a limited referral base can increase the efficiency of coordination tasks. Another physician said, “Within the laws of Medicare, our social workers must give people choices about home health care, but most turn around to ask the social worker who they would choose. We try to partner with a relatively small amount of high-quality home care agencies because it gives us better ability to communicate. our social worker can communicate once or twice a week with an analogous person on their end and go through 10 patients together. When it’s ‘onesie, twosie’ none of us make the commitment to go through it.”
Internists in two different integrated medical systems described their use of the EMR and secure e-mail for e-referrals. In some cases if the specialist is provided with sufficient information (attached photos, labs, diagnostic images), the patient does not need to actually have a visit with the specialist. Respondents noted that this helps keep care coordinated by the PCP, improves access to specialists, and improves efficiency of use of specialists’ time.
While not novel or a guarantee that coordination will occur, the co-location of primary care and specialist physicians was noted to facilitate coordination and patient compliance. Among respondents, one PCP explained his approach to co-locating with those specialists to whom he most commonly referred: “Patients are more likely to see a gastroenterologist in a familiar place then going to a new office.” A few large practices bring on-site select services, such as dieticians and audiologists, for their patients on a periodic basis. In rural areas, bringing the specialists to the local area on specific days was a strategy that improved coordination by the PCP, enhanced convenience and minimized patient travel.
Two respondents discussed the value of establishing PCP-specialist service agreements for care coordination. The goal of such agreements is to improve patient access to specialists, to identify when co-management of patients is necessary, to clearly outline expectations of each provider, and to ensure appropriate information flow between providers. As a PCP in Ferndale, Wash., described it, “We have to have those conversations and reach mutual agreements, or we’re continually putting the patient in the middle.”
Describing these agreements, the PCP said, “We have literally developed written, signed agreements with consultants around how we are going to coordinate care with the idea of creating warm handoffs, a seamless system. Generally the content has been partly about access. how to access the specialist quickly [for an urgent patient]. Then for routine visits, the second piece is information exchange, how can we be sure when you see the patient you know why they’re there and what we’re expecting of the consultation?”
The contents of the agreements differ by specialist type; but, “they all have the same components on how to communicate and refer back to the primary care physician,” including for new problems or abnormal lab results a specialist might identify that are outside of the specialist’s area of expertise. This helps avoid cross-referrals from one specialist to another for things that the patient’s PCP might be better positioned to address given their knowledge of the patient.
To initiate and establish these agreements, one model described involved a PCP representing her entire group in negotiations with a counterpart from a specialty group, with both practice managers present. Respondents noted that service agreements require consensus on the role of the PCP and frequent updates to ensure parties’ needs are met. In areas with multiple small practices, the establishment of service agreements can be a particular challenge, as another physician noted, “The challenge is that you just can’t have every group having a separate conversation with every other group, at some point it has to happen at the community level with medical staff aggregating.”
Practices with referral tracking systems used simple electronic databases or paper tracking. Important components of the referral tracking noted by respondents included:
Regardless of strategies used, facilitators of between-office coordination included a well- constructed referral note, effective phone communication between providers, and enlisting patient assistance in information transfer. Whether transmitted electronically or by paper, key components of the referral note cited by respondents include:
In some cases, physicians enlist the help of the patient in transferring information to a specialist. In an effort to keep a patient’s other active specialists in the loop, some will send those specialists a copy of the patient’s annual exam via the patient. As one physician said, “I encourage my patients to file their annual exam, which includes their medications and problem list, and I encourage them to take it to their visits with other doctors. I also routinely send a copy of their annual exam to the other important subspecialists [they see].”
Approaches to coordinating care between the hospital and the primary care practice ranged from primary care physicians admitting their own patients to programs that assist in coordination between settings.
Some of the primary care physicians interviewed provided inpatient care. “We try to provide seamless care for people. I am still one of the few physicians that sees patients in the clinic and the hospital, which makes it easier [to coordinate care] because when people go to the hospital, I control their whole hospitalization and who they and I refer to.” One primary care physician described a committee to work with a hospital to overcome the assumption that hospitalists will care for all admitted patients: “We’ve had to work hard to overcome the hospitalist culture, that some of us still like to do our own admissions.”
A shared interest around coordination from the hospital side is clearly helpful. A physician at a small family medicine practice in Muskegon, Mich., described how the consolidation of hospital ownership is helpful when his primary care practice needs to identify which of its patients are hospitalized. “There are three hospitals in town owned by the same corporation. Every day, the people in the medical records section in our office go into the hospital system and query it for our patients. That will depend on how well the hospital tries to get the primary care physician entered into the system so the data gets back to the primary care doctors. They are really interested in coordination of care and having us know which patients are in the hospital,” he said.
The Middlesex PHO-like integrated system (described earlier) works closely with independent primary care practices in the community to provide transition care for patients prior to discharge. Describing their approach, an advance practice nurse said, “When a patient is discharged I’ll see them and set up a plan for our work. We try to make an appointment with the patient before they’re discharged, so if they’re discharged today we try to see them within two days. At that time we’ll send a note to the primary care provider and work with the patient and primary care provider after discharge.” Care is resumed by the patient’s primary care provider once transition is complete.
Three practices described their use of the Care Transitions Program developed by Eric Coleman15 for patients discharged from hospital to home or to skilled-nursing facilities. The Care Transitions Program involves a personal health record (PHR), a discharge preparation checklist, a patient self-activation and management session with a transition coach (geriatric nurse practitioner) and follow-up visits after discharge with that coach. The program focuses on helping the patient with medication self-management, use of the PHR, scheduling and completing follow-up visits with the primary care and/or specialist physicians, and building patient awareness of “red-flag” symptoms that their condition is worsening.
At Austin Regional Clinic, a joint program between ambulatory providers and a hospital involves large hospitalist and outpatient primary care groups that work together. A nurse coordinator and office manager located in the hospital under the hospitalists’ group, as well as a portal providing the hospitalist group with access to the outpatient EMR, assists with coordination of care for patients between the two settings.
A link with the hospital’s EMR, the quality of the call system that notifies a physician when a patient presents to the hospital, and shared incentives around coordination created by integrated delivery systems, were cross-cutting facilitators of coordination between the inpatient and outpatient settings.
While less common, a handful of practices described efforts to coordinate with community-based services at local health departments, schools, pharmacies and hospices. Often these efforts involved state or grant funding or required the resources of larger or university-affiliated practices. A physician in a small practice in Oregon described a statewide Web-based immunization registry built with funding from the state. Describing its benefits when patients see multiple providers, the physician said, “I use the current database every day. If a patient is visiting our practice for the first time, and we’re not sure they’ve had a hepatitis A vaccine, you can look it up.” A nurse in a small New Hampshire pediatric practice described their work with the state to hold patient educational sessions in their community on “Paying the Bills” and “Meeting Your Needs in a Maze of Services.”
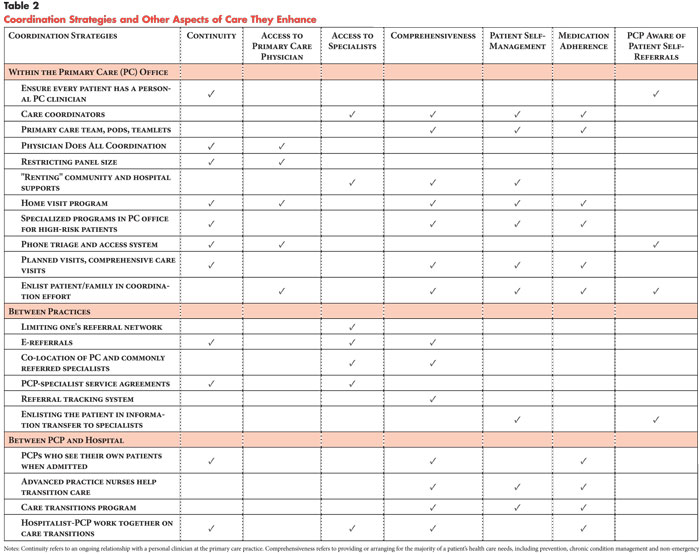
A pediatrician in a community health center described a work in progress to share care plans across a community of providers via a Web-based tool with “a standard intake assessment. . It’s not an EMR, but we could share care plans across the community.” Another physician in a university-affiliated practice described an interdisciplinary effort to make community resources more available to diabetics in their practice: “We paired with a pharmacist at a community-based pharmacy, a nutritionist in our hospital, and a social worker through the area agency on aging. In addition, there was an emphasis placed on activating the full practice staff as part of the participating team.” A respondent in a family practice network of 50 physicians described their efforts to improve coordination with hospice via the practice’s EMR, “We have given hospice in the county direct access to our EMR so they can type notes and route them to the doctor. We have a nursing home doing that as part of a pilot and that’s working well.” Finally, respondents often commented that strategies used to improve coordination of care also enhanced other aspects of care delivery (see Table 2).
![]() hile most practices did not systematically track the costs of their coordination efforts, their choices of strategies were directed toward making the services paid under fee-for-service operate more efficiently. For example, several practices that invested in coordination processes, such as channeling non-clinical coordination tasks to non-physicians, planned care visits and referral protocols, saw a positive impact on their bottom line “in the long run.” A physician described her practice’s improved efficiency as a result of the referral coordinator, “Patient encounters went up, definitely. There is less time on the phone, it’s easier to find referral information. that’s been helpful—less paperwork for me.”
hile most practices did not systematically track the costs of their coordination efforts, their choices of strategies were directed toward making the services paid under fee-for-service operate more efficiently. For example, several practices that invested in coordination processes, such as channeling non-clinical coordination tasks to non-physicians, planned care visits and referral protocols, saw a positive impact on their bottom line “in the long run.” A physician described her practice’s improved efficiency as a result of the referral coordinator, “Patient encounters went up, definitely. There is less time on the phone, it’s easier to find referral information. that’s been helpful—less paperwork for me.”
One practice saw a 50 percent drop in patient call volume once they began automatically renewing non-narcotic prescriptions for the full year at the time of the patient’s exam and thus avoided designating a full-time nurse to handle refill calls. Among practices that had adopted them, there was general consensus that at least one hour per day (in some cases two hours) of physician time were saved by moving to the team approach and doing planned care visits. This is consistent with a study that tracked office staff time spent in various activities.16
Office processes to improve care coordination can, nonetheless, require substantial investment of resources; for example, scheduling a call-in hour each morning for direct patient access to one’s physician cost a 13-physician group practice $875,000 a year, although the physicians realized the benefit of less-interrupted work throughout the day and improved coordination.
![]() espondents emphasized the need to reimburse care differently to enhance value for patients and providers in ways not captured in the context of existing fee-for-service arrangements, such as reduced ED visits and hospitalizations resulting from better coordination. Providers were universally adamant that they need payment for coordination efforts; a respondent said, “. you can’t talk about processes to improve coordination unless you value it.”
espondents emphasized the need to reimburse care differently to enhance value for patients and providers in ways not captured in the context of existing fee-for-service arrangements, such as reduced ED visits and hospitalizations resulting from better coordination. Providers were universally adamant that they need payment for coordination efforts; a respondent said, “. you can’t talk about processes to improve coordination unless you value it.”
In terms of how to reimburse providers for coordination activities, respondents were wary of creating “more little fee-for-service codes” since the burden of documentation could be “overwhelming.” One physician captured the sentiment of several respondents, “You can’t pay for this by dividing it into 50 different functions to document.” While some proposed a general incentive, such as a per-member, per-month payment, a few noted that failing to link payment to a specific goal or service would not necessarily create an incentive to perform time-intensive tasks needed to coordinate care.
As one national expert said, “I would do a fair amount of pay for performance based on patient scores of their care coordination.” Citing the benefits of capitation for coordination, one physician said, “If we were employed by a single entity that made care coordination a higher priority it would facilitate buy-in and investment, but we’re fragmented. If the payer recognized what we did to coordinate care outside the hospital as a valued service to be compensated, it would allow us to do a better job.”
![]() edical practices use a variety of strategies to coordinate care for patients both within the office and across providers and settings. Among respondents, coordination strategies were more focused on care within the office than across practices, most likely because of the lack of reimbursement for such activities.
edical practices use a variety of strategies to coordinate care for patients both within the office and across providers and settings. Among respondents, coordination strategies were more focused on care within the office than across practices, most likely because of the lack of reimbursement for such activities.
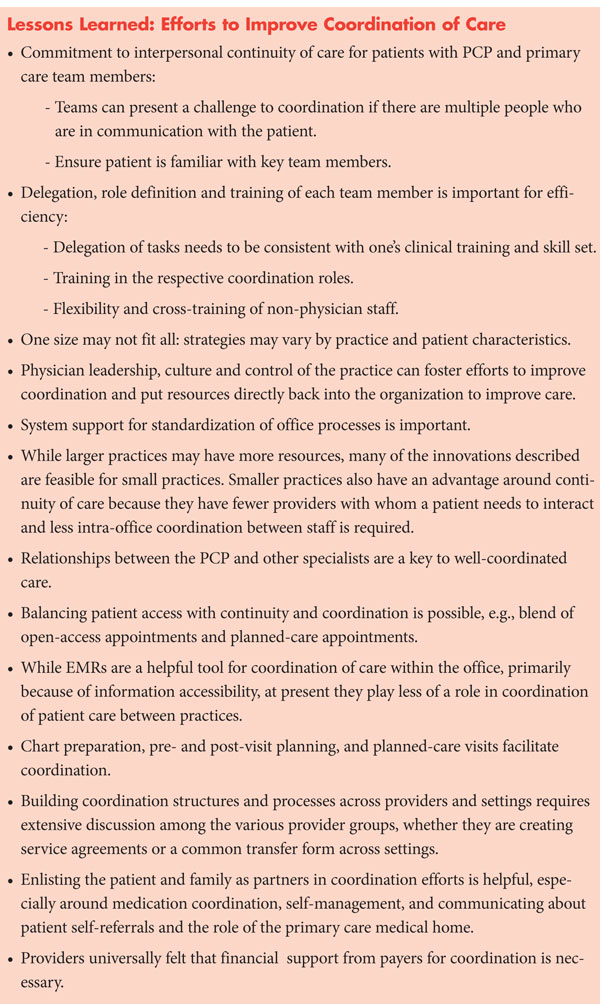
While there is no single recipe for care coordination given the range of patient, physician, practice and local market factors, some cross-cutting lessons can be identified from respondents’ experiences, such as the value of a commitment to interpersonal continuity of care as a precursor for coordination (see box). The importance of system support for the standardization of office processes also was identified by respondents as fostering coordination. A lead clinician’s buy in was similarly identified as necessary to establishing standardized processes.
Even though larger practices may have more resources to invest, many of the innovations respondents described are possible for small practices and could be scaled to an individual practice’s resources. In fact, respondents believed that such tools as pre-visit planning use less staff resources overall once the practice has established the pattern. Smaller practices also seemed to have less of a challenge with interpersonal continuity, given fewer staff with whom a patient must interact.
Respondents were nearly universal in noting that working relationships between the PCP and other specialists are a key to well-coordinated care. According to one PCP, “The gastroenterologist has trust that I will send him the right patient with the right indication, that there will be no surprises, [that he will receive from me the patient’s] list of medications and allergies. It is cost and time saving for the patient and saves time for us.” Like others, he noted that such working relationships help physicians of all specialties to maximize efficiency given time pressures.
Finally, building coordination structures and processes that work across providers requires extensive discussion among provider groups. For example, two respondents who believed they had made “enormous progress” with service agreements, nonetheless, described the dialogue as “ongoing work.” The value, however, lies in the enhanced understanding of each provider’s issues and the ability to communicate about patient care.
![]() he clinical effectiveness of a few of the strategies respondents
mentioned has been empirically tested. For example, the use of advance practice
nurses to ease care transitions from inpatient to outpatient settings has been
demonstrated to reduce re-admission rates for congestive heart failure patients.17
The potential of primary care teams and planned visits have been identified
by others as highly promising,13,14,18,19
but their impact on outcomes has received less attention. Similarly, the strategy
of “renting services” from outside the primary care office to work closely with
the PCP has been described in a case study.20 Early results
from a randomized controlled trial of the Guided Care Model, in which a registered
nurse, intensively trained in chronic care, works with physicians in primary
care practices to provide coordinated and comprehensive chronic care, are also
positive.21
he clinical effectiveness of a few of the strategies respondents
mentioned has been empirically tested. For example, the use of advance practice
nurses to ease care transitions from inpatient to outpatient settings has been
demonstrated to reduce re-admission rates for congestive heart failure patients.17
The potential of primary care teams and planned visits have been identified
by others as highly promising,13,14,18,19
but their impact on outcomes has received less attention. Similarly, the strategy
of “renting services” from outside the primary care office to work closely with
the PCP has been described in a case study.20 Early results
from a randomized controlled trial of the Guided Care Model, in which a registered
nurse, intensively trained in chronic care, works with physicians in primary
care practices to provide coordinated and comprehensive chronic care, are also
positive.21
This study’s findings in small practices were consistent with some findings from large practices of more than 200 physicians in mostly integrated health systems participating in the Medicare Physician Group Practice Demonstration (PGP).22 In particular, PGP participants identified delegation of some coordination tasks to non-physicians, standardization of particular care processes, the use of planned visits with pre-visit preparation and the importance of physician leadership in change processes as important to improve coordination of care. The PGP demonstration sites found teamwork helpful in improving quality and efficiency. Moreover, unlike respondents in this study, the PGP participants had additional financial incentives to pursue their practice redesign efforts, and since all were large, they had more resources at their disposal. Common findings between the PGP demonstration and this study in smaller practices highlight particular strategies with the most potential for sustainability.
Many of the strategies described are good candidates for more empiric examination. Practice-based research networks involving small to medium-sized practices could assess the impact of strategies on patient ratings of coordination, clinical outcomes and costs.
The limited number of examples of coordination between practices and community services was also notable. The few examples of such coordination with community services were either state funded or occurred in larger systems. Yet, collaboration between primary care and local community services is important, particularly for vulnerable patients.23 However, resources for smaller practices to help establish such linkages are limited, especially given the numerous demands they already face.
![]() hese findings have implications for physician payment, medical-home initiatives and technical support to practices, performance measurement, and practice referral networks. Some respondents’ coordination strategies resulted in improved efficiency over time for practices, but by and large, practices currently pursue these efforts at their own expense. One of the goals of current medical-home experiments is to begin to address the lack of reimbursement for coordination efforts.
hese findings have implications for physician payment, medical-home initiatives and technical support to practices, performance measurement, and practice referral networks. Some respondents’ coordination strategies resulted in improved efficiency over time for practices, but by and large, practices currently pursue these efforts at their own expense. One of the goals of current medical-home experiments is to begin to address the lack of reimbursement for coordination efforts.
The variation in practices’ strategies has implications for medical-home initiatives in terms of measuring coordination capabilities. A medical home measurement tool used to qualify practices for additional payments will need to permit flexibility in how practices demonstrate that they coordinate care. At the same time, the tool needs to ensure that the various aspects of coordination, both within and across providers and settings, are measured.
Even if practices that participated in this study were potentially higher functioning than average practices, among these it is notable that there was a wide range of organizational and technical sophistication. Thus, efforts to provide technical support to practices to improve coordination need to consider the baseline from which more typical practices may be starting, and tailor their support to practices ranging widely in size, resources, and existence of standardized care processes. They will also likely need to encourage less tangible factors, such as leadership, that respondents believed were critical to improving coordination processes.
In terms of performance measurement, a few respondents were motivated to adopt the coordination strategies they used after participating in American Board of Internal Medicine and National Committee on Quality Assurance quality improvement efforts focused on a single condition, such as diabetes care. The reverse may also be true, i.e., including in performance measurement assessments of whether primary care practices have coordination structures and processes in place is likely to improve clinical outcomes across a range of conditions. Public reporting also was cited as a motivator by physicians, thus incorporation of coordination measures reflecting patient satisfaction with coordination of care might help create incentives for coordination.
Patients often look to their PCP for referral recommendations.24 And, PCPs clearly gravitate toward keeping their referral networks to a manageable size to foster familiarity, trust and working relationships. The reality however is that providers face many different health plan referral networks. Assisting PCPs by the provision of quality data on specialists (not just in terms of their adherence to process measures or costs, but in terms of their accessibility and communication with the PCP) might foster referrals in a way that enhances coordination.
Lessons learned from some of the approaches described may help facilitate coordination in other practices. If aligned with payment incentives, some of these strategies have potential to increase quality and satisfaction among patients and providers by helping to move the health care delivery system toward better coordinated care.
A total of 62 respondents were interviewed for this study between December 2007 and May 2008. Most were from practices responding to announcements about this study posted on membership listservs for the American College of Physicians (ACP) and the American Academy of Family Practice (AAFP). The listserv announcements invited practices that “were doing innovative and/or effective things to coordinate patients’ care.” Additional references were obtained from the seven national experts interviewed in the first phase of the study, the American Board of Internal Medicine (ABIM), TransforMED and the Council of Accountable Physician Practices (CAPP).
A physician was interviewed from each practice. In cases where that physician believed a second respondent could provide additional insights and perspectives on care coordination efforts within the practice, a second respondent was interviewed, most often an R.N., referral coordinator or practice manager.
Each interview was conducted using a two-person team. The semi-structured interview protocols were informed by established primary care and care coordination conceptual frameworks.8-10 Interview notes were transcribed, jointly reviewed, coded and then analyzed using Atlas.ti qualitative software.
After queries about practice and panel characteristics, respondents were
asked about each of the following: 1) How does your practice coordinate care
for patients, both within and across practices and settings? 2) What are the
barriers to and facilitators of coordination, both within a primary care practice
and across various providers and settings? 3) What are the lessons learned that
might be applied in other settings that are not currently coordinating care
well? and 4) How has the institution of these care processes affected the practice’s
financial bottom line?
This research was funded by the Robert Wood Johnson Foundation’s Changes in Health Care Financing and Organization Initiative, which is administered by AcademyHealth. Special thanks go to the American College of Physicians (ACP), the American Academy of Family Physicians (AAFP), TransforMED (Transforming Medical Practices), the American Board of Internal Medicine (ABIM) and Council of Accountable Physician Practices (CAPP) for helping to identify and contact practices with innovative approaches to care coordination.We are grateful to the anonymous practice and national expert respondents who gave so generously of their time for interviews.
RESEARCH BRIEFS are published by the Center for Studying Health System
Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org