
Issue Brief No. 106
November 2006
Joy M. Grossman, Marie C. Reed
Physicians in smaller practices continue to lag well behind physicians in larger practices in reporting the availability of clinical information technology (IT) in their offices, according to a new national study from the Center for Studying Health System Change (HSC). The proportion of physicians reporting access to IT for each of five clinical activities increased across all practice settings between 2000-01 and 2004-05. Adoption gaps between small and large practices persisted, however, for two of the clinical activities—obtaining treatment guidelines and exchanging clinical data with other physicians—and widened for the other three—accessing patient notes, generating preventive care reminders and writing prescriptions. In contrast, clinical IT was generally as likely or more likely to be available to physicians in practices treating larger proportions of vulnerable and underserved patients as other physicians, a pattern that did not change between the two periods.
![]() arger physician practices, including group/staff model
health maintenance organizations (HMOs), medical school faculty practices and
large groups, have been the earliest adopters of clinical IT. While overall
IT adoption has grown slowly, policy makers are particularly concerned about
how IT is diffusing among small practices and physicians serving rural, low-income
or minority patients.1
arger physician practices, including group/staff model
health maintenance organizations (HMOs), medical school faculty practices and
large groups, have been the earliest adopters of clinical IT. While overall
IT adoption has grown slowly, policy makers are particularly concerned about
how IT is diffusing among small practices and physicians serving rural, low-income
or minority patients.1
More than half of all physicians in 2004-05 worked in solo and two physician practices (32%) or small groups of three to nine physicians (19%), according to HSC’s nationally representative Community Tracking Study (CTS) Physician Survey (see Data Source). Small and safety net practices may be left behind even as adoption accelerates among larger practices, widening the adoption gaps and, potentially, disparities in the quality of care among patients.
Recent findings from the CTS Physician Survey show that the percentage of physicians reporting access to IT for each of five clinical activities—obtaining treatment guidelines, exchanging clinical data with other physicians, accessing patient notes, generating preventive reminders for the physician’s use and writing prescriptions—grew between 2000-01 and 2004-05 across all practice settings (see Table 1). However, adoption gaps between physicians in smaller and larger practices persisted over the same period.
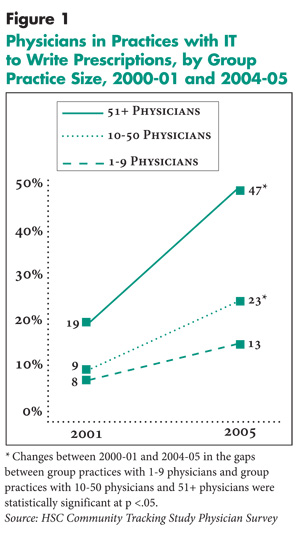
The adoption gap between physicians in the smallest practices (with nine or fewer physicians) and physicians in large group practices (with more than 50 physicians) grew for three of the five activities: accessing patient notes, generating preventive care reminders and writing prescriptions. As an example, the proportion of physicians in the smallest practices reporting IT to write prescriptions increased 5 percentage points over the period, while the proportion of physicians in large groups grew by 28 percentage points (see Figure 1). As a result, the adoption gap tripled between 2000-01 and 2004-05. Adoption gaps between physicians in the smallest practices and large groups leveled out for accessing guidelines and exchanging clinical data (with any increases in the gaps not statistically significant). Widening gaps were also reported between physicians in the smallest practices and those in the middle group of practices with 10 to 50 physicians for all clinical activities but reminders.
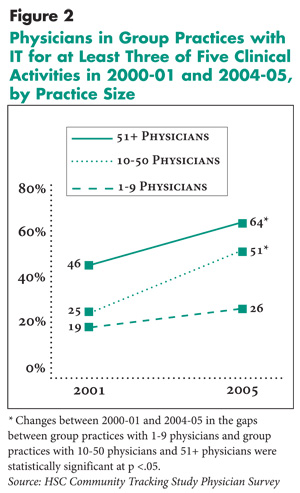
A similar pattern existed among high-adopting practices with the most IT (see Figure 2). For example, among physicians reporting that IT is available for three or more of the five clinical activities, the gaps between those in the smallest practices and large groups increased by 40 percent.
Practice size gaps may be explained by factors such as larger practices’ greater financial and administrative resources, scale economies—the ability to spread acquisition and implementation costs among more physicians—and more active physician leadership promoting IT and quality improvement.
Adoption gaps also persisted by physician specialty and age for all clinical activities. The gaps were smaller, however, than practice size differences in adoption and did not widen over the four-year period.
Table 1
|
||||||||||
|
|
Obtain Guidelines
|
Exchange Clinical Data
|
Access Patient Notes
|
Generate Reminders
|
Write Prescriptions
|
|||||
|
2001
|
2005
|
2001
|
2005
|
2001
|
2005
|
2001
|
2005
|
2001
|
2005
|
|
| All Physicians |
53%
|
65%#
|
41%
|
50%#
|
37%
|
50%#
|
24%
|
29%#
|
11%
|
22%#
|
| Practice Size | ||||||||||
| Solo/2 Physicians |
47*
|
54*#
|
25*
|
29*#
|
24*
|
31*#
|
23
|
25*
|
7*
|
12*#
|
| 3-9 Physicians |
54
|
62#
|
35*
|
43*#
|
30*
|
40*#
|
24
|
28*#
|
10*
|
14*#
|
| 10-50 Physicians |
48*
|
68#
|
42*
|
61*#
|
40*
|
56*#
|
21*
|
27*#
|
9*
|
23*#
|
| 51+ Physicians |
57
|
65
|
62
|
73#
|
55
|
79#
|
28
|
40#
|
19
|
47#
|
| Medical School |
66*
|
79*#
|
72*
|
81#
|
66*
|
79#
|
20*
|
34#
|
15
|
31*#
|
| Group/Staff HMO |
76*
|
90*#
|
75*
|
83*#
|
83*
|
85
|
59*
|
65*
|
38*
|
59*#
|
| Hospital Staff |
55
|
70#
|
49*
|
54*
|
41*
|
60*#
|
19*
|
24*#
|
14*
|
26*#
|
| Specialty | ||||||||||
| Primary Care |
53*
|
66#
|
35*
|
44*#
|
32*
|
47*#
|
26*
|
35*#
|
12
|
25#
|
| Medical Specialist (R) |
58
|
69#
|
47
|
56#
|
43
|
57#
|
19
|
23#
|
12
|
23#
|
| Surgical Specialist |
46*
|
57*#
|
39*
|
50*#
|
36*
|
46*#
|
26*
|
30*
|
9
|
17*#
|
| Age | ||||||||||
| Younger than 35 |
57
|
75*#
|
43
|
52#
|
37
|
58#
|
22
|
28#
|
13
|
24#
|
| 35 to 54 (R) |
55
|
67#
|
42
|
53#
|
38
|
53#
|
23
|
30#
|
12
|
25#
|
| 55 and Older |
45*
|
58*#
|
34*
|
43*#
|
32*
|
42*#
|
24
|
28#
|
9*
|
15*#
|
| Location | ||||||||||
| Metropolitan (R) |
53
|
65#
|
41
|
51#
|
37
|
51#
|
23
|
30#
|
11
|
22#
|
| Nonmetropolitan |
56
|
64#
|
33*
|
42*#
|
33
|
45*#
|
25
|
27
|
10
|
19#
|
| Medicaid Revenue | ||||||||||
| <25% of Practice Revenue (R) |
52
|
64#
|
39
|
50#
|
35
|
49#
|
24
|
30#
|
11
|
22#
|
| >25% of Practice Revenue |
56*
|
67#
|
46*
|
50
|
44*
|
55*#
|
23
|
27
|
12
|
23#
|
| Note: Nonmetropolitan areas include micropolitan
and rural areas. Micropolitan areas, as defined by the White House Office
of Management and Budget, are generally nonmetro counties with an urban
area between 10,000 and 50,000 in population or that meet specified commuting
criteria to an urban area. For purposes of this analysis, rural areas are
generally nonmetro counties that do not meet the micropolitan definition. * Difference from reference group, as indicated by (R), is statistically significantly at p<.05. # Change from 2000-01 is statistically significant at p<.05. Source: Community Tracking Study Physician Survey |
||||||||||
 |
 |
![]() n 2004-05, as four years before, the relationship between
practice size and IT adoption was more pronounced for some clinical activities
than others. There were direct increasing relationships between size and IT
adoption to exchange clinical data and access patient notes and, to a lesser
extent, obtain guidelines. The pattern of adoption differed for preventive reminders
and writing prescriptions, which had the lowest overall adoption rates. The
percentage of physicians reporting IT in their practice for these activities
varied much less by practice size, particularly among practices with 50 or fewer
physicians.2 Physicians in large medical school faculty
practices also were less likely than physicians in groups of more than 50 to
report access to IT for these two activities in contrast to the other three.
n 2004-05, as four years before, the relationship between
practice size and IT adoption was more pronounced for some clinical activities
than others. There were direct increasing relationships between size and IT
adoption to exchange clinical data and access patient notes and, to a lesser
extent, obtain guidelines. The pattern of adoption differed for preventive reminders
and writing prescriptions, which had the lowest overall adoption rates. The
percentage of physicians reporting IT in their practice for these activities
varied much less by practice size, particularly among practices with 50 or fewer
physicians.2 Physicians in large medical school faculty
practices also were less likely than physicians in groups of more than 50 to
report access to IT for these two activities in contrast to the other three.
These differences in adoption gaps suggest that such factors as high costs and complexity that can be mitigated by larger practice size may be more direct drivers of adoption for some technologies, such as electronic medical records (EMRs) that allow physicians to access patient notes. The relatively flatter rates of adoption among physicians in most practice settings for other clinical activities may reflect that those adoption decisions are influenced by factors beyond cost. For example, preventive reminders may be a more clinically appropriate tool for some specialties than others, resulting in lower adoption across all practices sizes.
![]() hysicians in practices treating more underserved patients
were generally no less likely to report access to IT in their practices than
other physicians. For example, physicians in practices with the highest proportions
of Medicaid revenue (greater than 25% of total practice revenue) were as likely
or more likely than other physicians to report IT for each of the clinical activities
in both 2000-01 and 2004-05.They also were more likely to report being in high-adopting
practices with IT for three or more of the five clinical activities, although
the difference was not significant in 2004-05.3
hysicians in practices treating more underserved patients
were generally no less likely to report access to IT in their practices than
other physicians. For example, physicians in practices with the highest proportions
of Medicaid revenue (greater than 25% of total practice revenue) were as likely
or more likely than other physicians to report IT for each of the clinical activities
in both 2000-01 and 2004-05.They also were more likely to report being in high-adopting
practices with IT for three or more of the five clinical activities, although
the difference was not significant in 2004-05.3
These high Medicaid providers were as likely or more likely to have access to IT regardless of practice size (data not shown). Physicians in high Medicaid practices work in a variety of settings. In 2004-05, while almost 50 percent of these physicians were in settings traditionally thought of as safety net providers, such as medical school faculty practices, hospitals, community health centers (CHCs) or other clinics, another 37 percent were in solo and two physician practices (21%) and practices with three to nine physicians (16%). Even when looking only at smaller practices, where having a high Medicaid patient load could present even greater financial barriers to adoption, physicians with high Medicaid revenues were no less likely to report IT than their peers.
Access to IT was lower than average, however, for physicians in CHCs for two of the five clinical activities—exchanging clinical data and accessing patient notes. For these activities, CHC physicians report adoption rates similar to physicians in solo and two physician practices. CHC physicians also were no more likely to report that they were in high-adopting practices. The differences again likely highlight the importance of financial barriers to IT adoption for these two clinical activities.
Physicians in practices with the highest proportions of patients with chronic conditions and minority patients were as likely or more likely as other physicians to report having access to IT for all five clinical functions in 2004-05 (see Table 2). Questions about chronic conditions and patient race were not asked in the 2000-01 survey, but these findings are consistent with a previous HSC analysis that linked the CTS physician survey to Medicare beneficiary claims data to look at variation in access to IT by patient characteristics.4
There were some urban-rural adoption gaps. Physicians in nonmetropolitan areas reported somewhat lower rates of IT for exchanging clinical data and accessing patient notes but not for the other three clinical activities.5 They were also somewhat less likely to be in high-adopting practices.6 Location was no longer statistically significant once practice size and other factors were taken into account. These location gaps did not increase over the four-year period.
Table 2
|
|||||
|
Obtain Guidelines
|
Exchange Clinical Data | Access Patient Notes | Generate Reminders |
Write Prescriptions
|
|
| Patients with Chronic Conditions | |||||
| <80% of Patients (R) |
63%
|
47%
|
48%
|
30%
|
22%
|
| >80% of Patients |
69*
|
59*
|
58*
|
28
|
23
|
| Black Patients | |||||
| <30% of Patients (R) |
65
|
50
|
49
|
30
|
21
|
| >30% of Patients |
65
|
51
|
55*
|
27
|
24
|
| Hispanic Patients | |||||
| <20% of Patients (R) |
63
|
50
|
49
|
29
|
22
|
| >20% of Patients |
70*
|
51
|
53
|
30
|
23
|
| * Difference from reference group, as indicated
by (R), is statistically significantly at p<.05. Source: Community Tracking Study Physician Survey |
|||||
![]() ccess to clinical IT is growing across all practice settings and all types of physicians. Clinical IT has diffused widely among practices most likely to be early adopters, including group/staff model HMOs, medical school faculty practices and group practices of more than 50 physicians, at least for selected clinical activities. A large majority of physicians in these large practices now have access to IT for treatment alternatives, exchanging clinical data and accessing patient notes, with preventive reminders and writing prescriptions lagging somewhat.
ccess to clinical IT is growing across all practice settings and all types of physicians. Clinical IT has diffused widely among practices most likely to be early adopters, including group/staff model HMOs, medical school faculty practices and group practices of more than 50 physicians, at least for selected clinical activities. A large majority of physicians in these large practices now have access to IT for treatment alternatives, exchanging clinical data and accessing patient notes, with preventive reminders and writing prescriptions lagging somewhat.
However, adoption gaps between smaller and larger groups continue to exist and are widening for some clinical activities—a concern given that the majority of physicians work in these smaller practices. The differences may reflect a natural path of technology adoption where larger, savvier organizations adopt new technologies first and others follow, albeit at a slower rate. Or it may be that smaller practices face different and substantial barriers that affect how quickly they catch up, if ever. The findings suggest that while in the aggregate, physicians in practices treating the underserved do not lag behind significantly in access to IT, critical groups of safety net providers, such as CHCs, also likely face large adoption barriers. Many public and private efforts are underway to help speed adoption of IT in the ambulatory setting. However, right now activities specifically targeted at small practices or the safety net are not widespread.
This Data Bulletin presents findings from the HSC Community Tracking Study Physician Survey, a nationally representative telephone survey of physicians involved in direct patient care in the continental United States conducted in 1996-97, 1998-99, 2000-01 and 2004-2005. The sample of physicians was drawn from the American Medical Association and the American Osteopathic Association master files and included active, nonfederal, office- and hospital-based physicians who spent at least 20 hours a week in direct patient care. Residents and fellows were excluded. Questions on information technology were added to the 2000-01 survey and continued in the 2004-05 survey. The 2000-01 survey contains information on about 12,000 physicians, while the 2004-05 survey includes responses from more than 6,600 physicians. The response rates were 59 percent in 2000-01 and 52 percent in 2004-05. More detailed information on survey methodology can be found at www.hschange.org.
Physicians were asked, “In your practice, are computers or other forms of information technology used: (1) to obtain information about treatment alternatives or recommended guidelines, (2) for clinical data and image exchanges with other physicians, (3) to access patient notes, medication lists, or problems, (4) to generate reminders for you about preventive services, and (5) to write prescriptions,” among other clinical activities. The survey data should be considered an upper limit on the percentage of physicians who regularly use IT since physicians were not asked whether or how often they themselves use it. The survey did not assess the use of specific technologies. For example, physicians can access electronic patient notes through a variety of mechanisms, such as an electronic medical record (EMR), practice management system, or Web-based portal. And a given application, such as an EMR, can support some or all of the clinical activities.
ISSUE BRIEFS are published by the
Center for Studying Health System Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org