
Issue Brief No. 56
October 2002
Ashley C. Short, Cara S. Lesser
![]() ising premiums and a weak economy are generating questions about the potential
erosion of health insurance coverage, particularly for the more than 46 million
Americans who work for small firms.1 People working in small firms typically have
less access to coverage than those in large firms. In 2000 and early 2001, the Center
for Studying Health System Change (HSC) conducted its third round of site visits to
12 nationally representative metropolitan areas2
and found that while few small employers actually dropped coverage, many increased the employee share of premiums,
raised copayments and deductibles, switched products and carriers and/or
reduced benefits. With the U.S. economy now in rougher shape, small employers
may pare back coverage even more, putting affordable health care further out of the
reach of workers and their families.
ising premiums and a weak economy are generating questions about the potential
erosion of health insurance coverage, particularly for the more than 46 million
Americans who work for small firms.1 People working in small firms typically have
less access to coverage than those in large firms. In 2000 and early 2001, the Center
for Studying Health System Change (HSC) conducted its third round of site visits to
12 nationally representative metropolitan areas2
and found that while few small employers actually dropped coverage, many increased the employee share of premiums,
raised copayments and deductibles, switched products and carriers and/or
reduced benefits. With the U.S. economy now in rougher shape, small employers
may pare back coverage even more, putting affordable health care further out of the
reach of workers and their families.
![]() he rising cost of health insurance
has led small employers to
make important changes in the health
insurance they offer their workers.
Insurance premiums rose rapidly for
all firms in 2000 and 2001, but small
firms were hit particularly hard, with
an average hike of 14.5 percent in
2001 (see Figure 1).
he rising cost of health insurance
has led small employers to
make important changes in the health
insurance they offer their workers.
Insurance premiums rose rapidly for
all firms in 2000 and 2001, but small
firms were hit particularly hard, with
an average hike of 14.5 percent in
2001 (see Figure 1).
Large employers generally made only modest changes to their insurance offerings in response to rising premiums, such as altering cost sharing.3 But small firms often have more difficulty than larger employers in affording health insurance for their workers (see box). Indeed, small employers in most of the 12 sites studied took more dramatic action, including:
Although the extent to which employers adopted these strategies varied (see Figure 2), the overall trend suggests that people working for small firms were beginning to face a greater financial burden for their health care costs—even at a time when the economy was relatively strong.
Figure 1
Percent Increase in Premiums by Firm Size
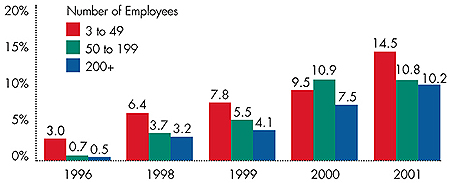
Source: The Kaiser Family Foundation and Health Research and Educational
Trust’s Employer Health Benefits Annual Survey
Figure 2
Number of Sites Reporting Changes in Small Employers’ Benefits Offerings
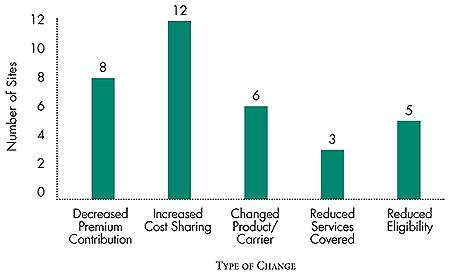
Source: Community Tracking Study site visits, 2000-01
![]() mall employers in more than half the
sites studied began shifting a greater
share of premiums to employees in
2000 and 2001. Many firms set their
premium contributions at a fixed percentage,
thus transferring some of the
burden of premium increases to
employees. Some small employers
decreased the percentage they contributed. In a few sites, some employers
went a step further and abandoned the fixed
percentage approach in favor of making a
fixed-dollar contribution, leaving employees
responsible for any premium costs above that
amount. This strategy shifted the premium
increases directly to employees.
mall employers in more than half the
sites studied began shifting a greater
share of premiums to employees in
2000 and 2001. Many firms set their
premium contributions at a fixed percentage,
thus transferring some of the
burden of premium increases to
employees. Some small employers
decreased the percentage they contributed. In a few sites, some employers
went a step further and abandoned the fixed
percentage approach in favor of making a
fixed-dollar contribution, leaving employees
responsible for any premium costs above that
amount. This strategy shifted the premium
increases directly to employees.
Another particularly troubling way small employers reduced their exposure to premium increases was to drop all contributions for dependent coverage. Such policies discouraged employees from covering their dependents and created the potential for adverse selection, since higher costs might deter healthier families from enrolling. In Miami, for instance, a broker reported that this trend was most pronounced in one- to 10-person firms, and that few employees of these firms elected dependent coverage as a result.
![]() mall firms in all 12 sites sought to minimize
premium increases by adding or increasing
deductibles, copayments and coinsurance.
These measures were intended to reduce the
current year’s premiums by placing a higher
cost burden on consumers who used services.
In addition, they potentially could rein in
utilization, thereby offsetting future increases.
mall firms in all 12 sites sought to minimize
premium increases by adding or increasing
deductibles, copayments and coinsurance.
These measures were intended to reduce the
current year’s premiums by placing a higher
cost burden on consumers who used services.
In addition, they potentially could rein in
utilization, thereby offsetting future increases.
For example, a Syracuse insurance broker reported that plans had added deductibles of $200 to $500 for hospital stays. In Boston, plans increased copayments for office visits from $5 to $10. And in Little Rock, Ark., some small employers raised coinsurance to as much as 40 percent or 50 percent.
Movement toward a three-tier prescription drug benefit was the most commonly reported change in out-of-pocket expenses. Under this scheme, consumers pay progressively more for generic drugs, preferred brand-name drugs and nonpreferred brand-name drugs. Some employers also replaced fixed dollar copayments with a percentage coinsurance, increasing workers’ costs even more.
![]() mall firms have more flexibility than large
firms to switch products and plans. As
premiums rose in 2000 and 2001, some
small employers moved to less expensive and
more restrictive product types to reduce net
increases in premiums. For example, some
employers in Orange County, Calif., moved
from preferred provider organizations (PPOs)
to point-of-service products, while in Cleveland
some switched from PPOs to health maintenance
organizations (HMOs).
mall firms have more flexibility than large
firms to switch products and plans. As
premiums rose in 2000 and 2001, some
small employers moved to less expensive and
more restrictive product types to reduce net
increases in premiums. For example, some
employers in Orange County, Calif., moved
from preferred provider organizations (PPOs)
to point-of-service products, while in Cleveland
some switched from PPOs to health maintenance
organizations (HMOs).
Other small employers found they could save on premiums simply by switching carriers. Some small employers routinely switched plans for even small cost savings, but with rapidly rising premiums, more found themselves shopping around for better deals.
While changes such as moving to more restrictive forms of coverage and switching health plans do maintain coverage, they exact a toll on consumers. Switching products or plans, particularly a move to managed care options, can disrupt relationships between patients and their physicians. For example, patients whose employers switch to HMOs may find their physicians do not participate in the plan, forcing them either to change doctors or to pay the full cost of their care.
![]() either small nor large employers relied
heavily on reductions in services covered to
counteract premium increases. In some communities,
however, small employers began to
chip away at their benefits offerings. Some
plans in Miami, for example, eliminated coverage
for fertility treatment, and small firms
in Indianapolis were considering whether to
reduce their coverage for mental illness.
either small nor large employers relied
heavily on reductions in services covered to
counteract premium increases. In some communities,
however, small employers began to
chip away at their benefits offerings. Some
plans in Miami, for example, eliminated coverage
for fertility treatment, and small firms
in Indianapolis were considering whether to
reduce their coverage for mental illness.
At the same time, large and small employers were reexamining their eligibility criteria. Large companies discussed dropping retiree coverage, as did some of the relatively few small firms offering such benefits. Small employers in several sites focused on other areas to scale back eligibility, establishing stricter rules for employees and dependents. For example, some small employers in Syracuse extended the waiting period for employee eligibility, and respondents in Phoenix and Boston predicted employers in those cities would adopt similar policies. Small employers in Miami and Greenville, S.C., went one step beyond eliminating the premium contribution for dependents and dropped dependent coverage entirely, creating concerns among policy makers about the increasing number of uninsured people in the area.
Despite speculation that employers would drop coverage altogether, there was little evidence of this during the 2000-01 site visits. One exception was Little Rock, where some small employers allowed employees to use pretax dollars to buy individual insurance. While employers sometimes use this approach to share the cost of individual coverage, the Little Rock firms required workers to bear the full cost of coverage in the more expensive individual market.
![]() ven in the thriving economy of 2000 and
early 2001, small employers’ responses to rising
premiums were making coverage and
care more expensive for workers and their
families. Increases in employees’ share of the
premium and tighter eligibility requirements
intensified the financial burden of purchasing
coverage. Meanwhile, increased cost sharing
and reductions in benefits strained the
pocketbooks of even those employees who
could afford coverage. Indeed, recent Census
Bureau data show a decline in the proportion
of individuals working in firms with fewer
than 25 employee who received coverage
through their employer in 2001.7
Rising premiums
also may have discouraged some
firms from beginning to offer coverage.
ven in the thriving economy of 2000 and
early 2001, small employers’ responses to rising
premiums were making coverage and
care more expensive for workers and their
families. Increases in employees’ share of the
premium and tighter eligibility requirements
intensified the financial burden of purchasing
coverage. Meanwhile, increased cost sharing
and reductions in benefits strained the
pocketbooks of even those employees who
could afford coverage. Indeed, recent Census
Bureau data show a decline in the proportion
of individuals working in firms with fewer
than 25 employee who received coverage
through their employer in 2001.7
Rising premiums
also may have discouraged some
firms from beginning to offer coverage.
A new, more burdensome round of premium increases has occurred since these site visits, as the U.S. economy has remained sluggish. With financial pressures building, small employers are likely to cut back even more on health insurance offerings. Some may continue to make the kind of changes observed in 2000 and 2001. Others may find they have exhausted their arsenal of cost-cutting mechanisms and decide to drop coverage altogether, exacerbating the national problem of the uninsured and feeding future cost increases.
![]() ealth insurance coverage generally
costs more for firms with fewer than
50 employees, and many have limited
resources to devote to health benefits.
For example, less than two-thirds (62%)
of small firms offered insurance in 2001,
compared with 97 percent of larger firms.4
Even when small firms offer insurance,
fewer employees enroll, possibly because
they typically earn lower wages than
employees of large firms.5
Indeed, one
study found that only 74 percent of
employees in firms with fewer than 10
employees enroll in their firms’ health
insurance offerings, compared with 84
percent of employees in firms with more
than 100 workers.6
ealth insurance coverage generally
costs more for firms with fewer than
50 employees, and many have limited
resources to devote to health benefits.
For example, less than two-thirds (62%)
of small firms offered insurance in 2001,
compared with 97 percent of larger firms.4
Even when small firms offer insurance,
fewer employees enroll, possibly because
they typically earn lower wages than
employees of large firms.5
Indeed, one
study found that only 74 percent of
employees in firms with fewer than 10
employees enroll in their firms’ health
insurance offerings, compared with 84
percent of employees in firms with more
than 100 workers.6
| 1. | U.S. Census Bureau, County Business Patterns, 2000. The U.S. Census Bureau defines small firms as those with between one and 49 employees. |
| 2. | For site visit methodology, see www.hschange.org. |
| 3. | Trude, Sally, et al., “Employer-Sponsored Health Insurance: Pressing Problems, Incremental Changes,” Health Affairs, Vol. 21, No. 1 (January/February 2002). |
| 4. | The Henry J. Kaiser Family Foundation and Health Research and Educational Trust, Employer Health Benefits: 2001 Annual Survey, The Henry J. Kaiser Family Foundation (2001). The Kaiser Family Foundation defines small firms as those with between three and 49 employees. |
| 5. | Oi, Walter Y., and Todd L. Idson, “Firm Size and Wages,” in O. Ashenfelter and D. Card, eds., The Handbook of Labor Economics, Volume III, Amsterdam: North-Holland (1999). |
| 6. | Cooper, Philip F., and Barbara Steinberg Schone, “More Offers, Fewer Takers for Employment-Based Health Insurance: 1987 and 1996,” Health Affairs, Vol. 16, No. 6 (November/December 1997). |
| 7. | U.S. Census Bureau, Health Insurance Coverage: 2001. |
ISSUE BRIEFS are published by the Center for Studying Health System Change.
President: Paul B. Ginsburg
Director of Public Affairs: Richard Sorian
Director of Site Visits: Cara S. Lesser
Editor: The Stein Group
For additional copies or to be added
to the mailing list, contact HSC at:
600 Maryland Avenue, SW
Suite 550
Washington, DC 20024-2512
Tel: (202) 554-7549
(for publication information)
Tel: (202) 484-5261
(for general HSC information)
Fax: (202) 484-9258
www.hschange.org